Introduction to Diabetic Neuropathy
Diabetic neuropathy is a type of nerve damage that can occur in individuals with diabetes. This condition arises due to prolonged high blood glucose levels, which can injure nerve fibers throughout the body. While diabetic neuropathy can affect various nerves, it most commonly impacts those in the legs and feet.
Imagine John, a 45-year-old man who has been managing his type 2 diabetes for over a decade. Recently, he started noticing a persistent tingling sensation in his feet, which sometimes turned into sharp, burning pain. These symptoms gradually worsened, leading to numbness and difficulty in feeling the ground beneath his feet. John also began to experience muscle weakness, making it challenging to walk or even stand for extended periods.
Concerned about these symptoms, John decided to consult his healthcare provider. After discussing his medical history and performing a physical examination, his doctor suspected diabetic neuropathy. Further tests, including nerve conduction studies and blood tests, confirmed the diagnosis. John’s experience is not uncommon; diabetic neuropathy affects nearly 50% of people with diabetes at some point in their lives.
The impact of diabetic neuropathy on someone’s life can be profound. The pain and discomfort associated with nerve damage can lead to sleep disturbances, reduced mobility, and an overall decline in the quality of life. Additionally, the numbness and loss of sensation increase the risk of injuries and infections, particularly in the feet, which can escalate to more severe complications if left untreated.
Understanding the basics of diabetic neuropathy is crucial for anyone managing diabetes. Recognizing early symptoms and seeking timely medical advice can help mitigate the effects and improve one’s quality of life. Through this guide, we aim to provide comprehensive information to help individuals like John navigate the challenges of diabetic neuropathy and take proactive steps toward better health.
How Nerves Work: The Basics
Nerves are the body’s communication network, transmitting signals between the brain, spinal cord, and other parts of the body. Think of nerves as electrical wires that carry messages in the form of electrical impulses. These messages allow us to move, feel, and react to our surroundings. The anatomy of a nerve is essential to its function, and it consists of several key components.
At the core of a nerve is the axon, a long, slender projection that conducts electrical impulses away from the nerve cell body. The axon is often surrounded by a myelin sheath, a fatty layer that acts like insulation around an electrical wire. This sheath helps increase the speed and efficiency of signal transmission. Without myelin, the signals would travel much slower, similar to how a frayed electrical wire might struggle to carry a current.
To visualize this, imagine a telephone wire. The wire itself is like the axon, carrying the signal from one point to another. The rubber coating around the wire is akin to the myelin sheath, ensuring the signal is delivered quickly and accurately. When the myelin sheath is damaged or the axon is impaired, the communication between the brain and body becomes disrupted, leading to various neurological issues.
An easy way to remember the key components of nerve function is the mnemonic “SAM”: Sensory, Axon, Myelin. Sensory nerves carry information from the body to the brain, axons transmit these signals, and myelin sheaths ensure the signals are fast and efficient. This simple rhyme can help recall the basics of nerve anatomy and physiology.
Understanding these fundamental aspects of how nerves work sets the stage for comprehending the complexities of conditions like diabetic neuropathy. With a grasp of nerve function, we can better appreciate the challenges and changes that occur when this system is compromised by diseases such as diabetes.
The Role of Diabetes in Neuropathy
Diabetes, a chronic condition characterized by high blood sugar levels, plays a significant role in the development of neuropathy. Neuropathy refers to nerve damage that occurs due to various factors, with diabetes being one of the most common causes. The connection between diabetes and neuropathy lies in the persistent elevation of blood sugar levels, which can lead to extensive nerve damage over time.
When blood sugar levels remain high for extended periods, it begins to affect the blood vessels that supply nourishment to the nerves. The process starts with sugar accumulating in these blood vessels, leading to a condition known as hyperglycemia. Hyperglycemia damages the small blood vessels, reducing their ability to deliver essential nutrients and oxygen to the nerves. Without proper nourishment, the nerves start to deteriorate, resulting in neuropathy.
Imagine the nerves as electrical wiring in a house. Just as damaged wiring can lead to flickering lights or power outages, damaged nerves can cause a range of symptoms, from tingling and numbness to severe pain. This damage primarily affects the peripheral nerves, which are responsible for transmitting signals between the central nervous system and the rest of the body.
To illustrate this process more vividly, consider this simple rhyme:
When sugar’s high and blood’s not right,The nerves will suffer, day and night.
Vessels weaken, nerves decay,Diabetic neuropathy comes to stay.
This rhyme encapsulates the essence of how prolonged high blood sugar levels lead to nerve damage in individuals with diabetes. The progressive nature of this condition highlights the importance of maintaining optimal blood sugar levels through proper medical management, diet, and lifestyle changes. By understanding the role of diabetes in neuropathy, individuals can take proactive steps to prevent or mitigate the impact of this debilitating complication.
Axon Degradation: What Happens to Nerves
Diabetic neuropathy is a condition that significantly affects the nervous system, primarily through the process of axon degradation. The axons, which are the long, thread-like extensions of nerve cells, play a crucial role in transmitting electrical signals from one part of the body to another. When a person has diabetes, prolonged high blood sugar levels can cause these axons to deteriorate, leading to a range of complications.
To understand this, imagine an axon as a garden hose. Under normal conditions, a garden hose efficiently carries water from the faucet to the plants. However, when exposed to harsh conditions such as extreme weather or constant pressure, the hose may become brittle, develop cracks, or even break. Similarly, in diabetic neuropathy, the elevated glucose levels act like harsh conditions for the axons. Over time, these high sugar levels cause oxidative stress and inflammation, leading to the weakening and eventual breakdown of the axons.
This degradation occurs in several stages, which can be remembered using the mnemonic “D.A.M.A.G.E.”:
D – Demyelination: The protective myelin sheath around the axon starts to erode.
A – Axonal swelling: The axon begins to swell due to accumulated damage.
M – Mitochondrial dysfunction: The energy-producing structures within the axons fail to function properly.
A – Axonal fragmentation: The weakened axons start to break apart.
G – Glial cell activation: Support cells in the nervous system become overactive, contributing to inflammation.
E – End-stage nerve damage: The axon is severely damaged, leading to the loss of nerve function.
This systematic deterioration severely impacts the ability of nerves to transmit signals, resulting in symptoms such as numbness, tingling, and pain. Understanding the process of axon degradation in diabetic neuropathy is crucial for recognizing the importance of managing blood sugar levels to prevent or slow down this debilitating condition.
Imagine the nerves in your body as electrical wires running through a complex network, transmitting signals that control everything from movement to sensation. Just as these wires need insulation to function properly, nerves are wrapped in a protective layer called the myelin sheath. This myelin acts as a form of insulation, ensuring that electrical signals are transmitted efficiently and accurately. When this protective layer gets damaged—a condition known as demyelination—the efficiency of signal transmission is severely compromised, leading to a myriad of neurological issues.
Demyelination can be compared to stripping away the insulation from electrical wires. Without this crucial layer, the wires are exposed, and the electrical signals can become erratic or even fail to reach their intended destination. In the context of diabetic neuropathy, this disruption can cause symptoms such as numbness, tingling, burning sensations, and muscle weakness. Over time, these symptoms can lead to significant difficulties in performing everyday tasks, such as buttoning a shirt, walking, or even holding a cup of coffee.
To better understand the impact of demyelination, consider the following practical example: Imagine trying to use a phone charger with a frayed cable. The exposed wires might still transmit a charge, but the connection would be unstable and unreliable. Similarly, nerves affected by demyelination struggle to send clear, consistent signals, resulting in the unpredictable and often debilitating symptoms of diabetic neuropathy.
Here’s a simple rhyme to help remember the concept:
“Myelin sheath, keep it tight, Without you, nerves can’t work right.
Signals lost and senses blurred, Demyelination—it’s the word.”
By visualizing nerves as insulated wires and understanding the critical role of the myelin sheath, it becomes easier to grasp how its damage can lead to significant and challenging symptoms in diabetic neuropathy. This fundamental knowledge can also aid in recognizing the importance of managing blood sugar levels to prevent or mitigate the effects of demyelination.
Living with Diabetic Neuropathy: Practical Tips and Management
Living with diabetic neuropathy can be challenging, but with the right strategies, it is possible to manage the condition effectively and improve quality of life. Here are some practical tips and management techniques that can help individuals cope with diabetic neuropathy.
Lifestyle Changes: Implementing certain lifestyle changes can significantly alleviate symptoms. Maintaining a healthy diet is crucial; focus on eating balanced meals rich in vegetables, lean proteins, and whole grains while minimizing sugar intake. Regular physical activity, such as walking, swimming, or yoga, can improve blood circulation and reduce neuropathic pain. Additionally, quitting smoking and limiting alcohol consumption are essential as these habits can exacerbate nerve damage.
Foot Care: Proper foot care is vital for those with diabetic neuropathy. Inspect your feet daily for any cuts, blisters, or swelling, and keep them clean and moisturized. Wear comfortable, well-fitted shoes to prevent injuries and consider using orthotic supports if necessary. Regular visits to a podiatrist can help in early detection and treatment of foot-related issues.
Medication and Treatment: Various medications can help manage pain and other symptoms associated with diabetic neuropathy. Over-the-counter pain relievers, prescription medications such as anticonvulsants and antidepressants, and topical treatments like capsaicin cream can be effective. Additionally, alternative therapies like acupuncture and physical therapy may provide relief. Always consult with a healthcare provider before starting any new treatment regimen.
Coping Strategies: Psychological support is as important as physical management. Joining support groups or seeking counseling can provide emotional relief and help you connect with others facing similar challenges. Stress management techniques such as mindfulness, meditation, and deep-breathing exercises can also be beneficial in managing symptoms.
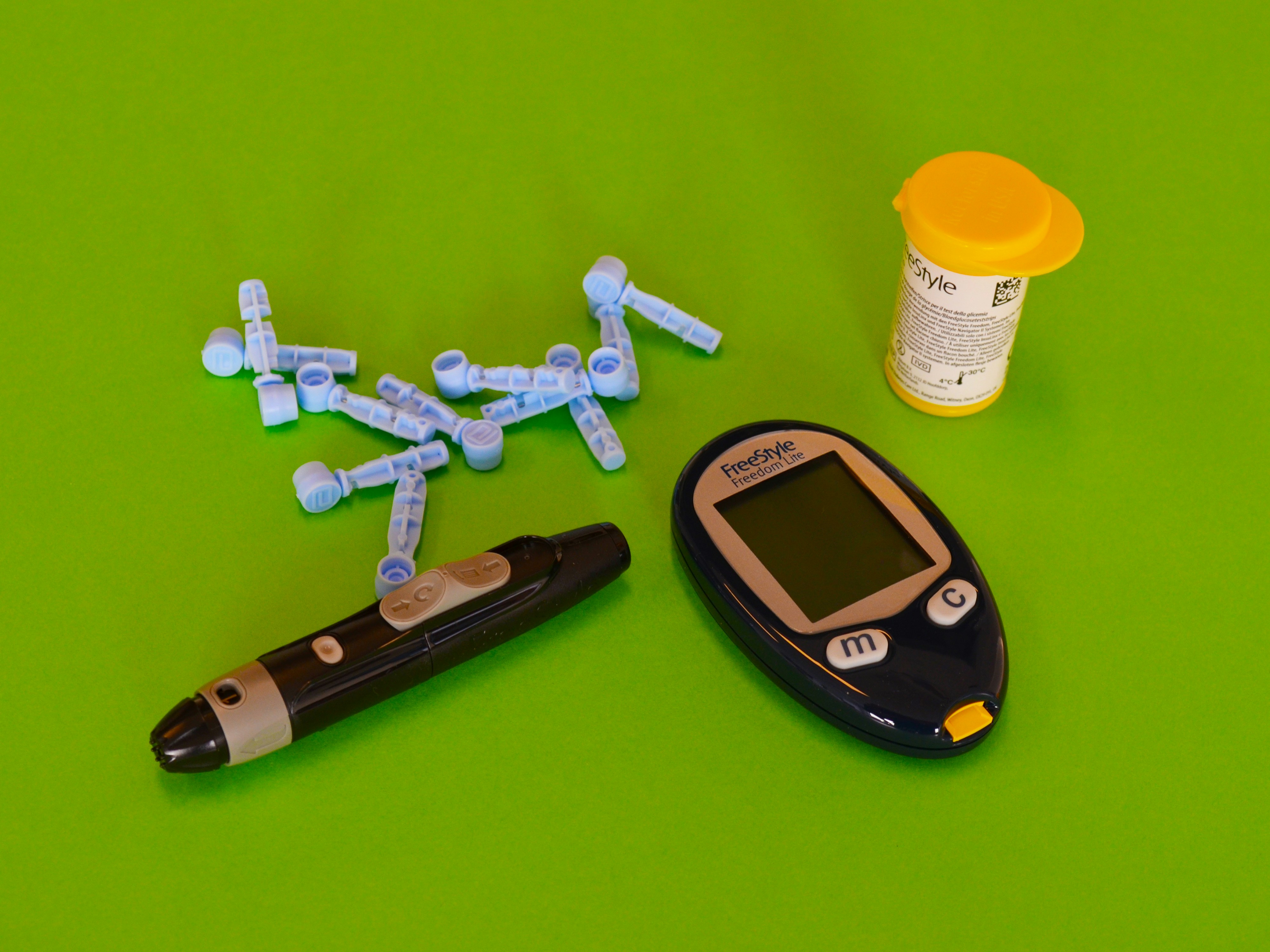
Monitoring Blood Sugar Levels: Keeping blood sugar levels within the target range is crucial for minimizing the progression of diabetic neuropathy. Regularly monitor your blood glucose levels, adhere to your diabetes management plan, and consult your healthcare team for adjustments as needed.
By integrating these practical tips into daily routines, individuals with diabetic neuropathy can better manage their symptoms and lead a more comfortable and fulfilling life.