Definition of Angina Pectoris
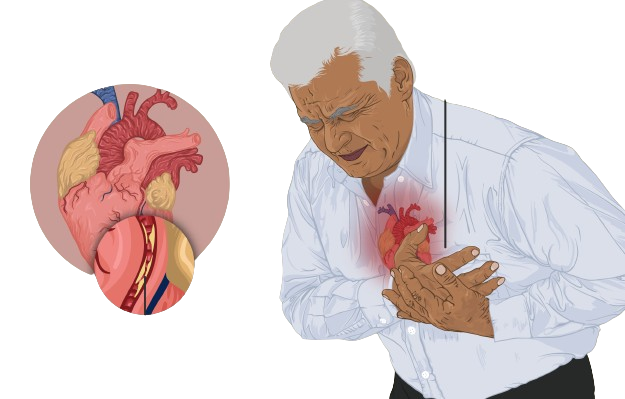
Angina Pectoris, often referred to simply as angina, is a medical condition characterized by chest pain or discomfort due to insufficient blood flow to the heart muscle. Essentially, it’s the heart’s way of signaling that it is not receiving an adequate supply of oxygen-rich blood. This condition manifests as a sensation of tightness, pressure, or squeezing in the chest, akin to having a tight band wrapped around the area. The discomfort may also radiate to other parts of the body, such as the shoulders, arms, neck, jaw, or back.
It is crucial to recognize that angina is not a disease in itself but rather a symptom indicative of an underlying cardiovascular issue, typically coronary artery disease (CAD). CAD occurs when the coronary arteries, which supply blood to the heart muscle, become narrowed or blocked due to the buildup of fatty deposits called plaques. This obstruction impedes the flow of blood, reducing the oxygen supply to the heart, which in turn triggers the pain or discomfort associated with angina.
Understanding the nature of angina is vital for timely diagnosis and management. The experience of angina can vary widely among individuals, with some describing it as a heavy weight on their chest, while others may feel it as a sharp or burning sensation. Regardless of the specific description, the common thread is the heart’s struggle for oxygen, prompting the need for medical attention to address the underlying cause and prevent potential complications.
By recognizing angina as a symptom of coronary artery disease, individuals can take proactive steps toward seeking appropriate medical care and making lifestyle changes to improve their heart health. Addressing risk factors such as smoking, high blood pressure, high cholesterol, and sedentary lifestyle can significantly mitigate the impact of CAD and, consequently, the occurrence of angina pectoris.
Signs and Symptoms of Angina Pectoris
Angina pectoris manifests in a variety of ways, with symptoms differing from person to person. The hallmark symptom is a sensation of pressure or squeezing in the chest. This discomfort can radiate to the shoulders, arms, neck, jaw, or back, creating a widespread feeling of unease. Many individuals liken it to carrying a heavy backpack throughout the day, resulting in aching shoulders and back. The chest pain associated with angina is often described as a heavy weight or a burning sensation.
Beyond chest pain, angina pectoris can present with additional symptoms. Shortness of breath is common, particularly during physical exertion or emotional stress. Sweating, nausea, and dizziness may also accompany the chest discomfort, further complicating the clinical picture. These symptoms can be alarming and are often indicative of underlying cardiovascular stress.
A useful mnemonic to remember the key aspects of angina pectoris is ‘PQRST’:
- Pain (chest): The primary symptom is chest pain or discomfort.
- Quality (pressure/burning): The pain is typically described as pressure or a burning sensation.
- Radiation (spreading to other parts): The discomfort can radiate to the shoulders, arms, neck, jaw, or back.
- Symptoms (shortness of breath, sweating): Accompanying symptoms may include shortness of breath, sweating, nausea, and dizziness.
- Timing (comes on with exertion): Symptoms often arise during physical activity or emotional stress and subside with rest.
Recognizing these signs and symptoms is crucial for early detection and management of angina pectoris. Understanding the varied presentations can help individuals seek timely medical advice and reduce the risk of more severe cardiovascular events.
Causes of Angina Pectoris
The primary cause of angina pectoris is reduced blood flow to the heart muscle, a condition often attributable to the buildup of fatty deposits known as atherosclerosis in the coronary arteries. This can be likened to a garden hose with a kink, where the water flow is significantly diminished. Similarly, when these arteries are narrowed or blocked, the heart muscle doesn’t receive adequate oxygen-rich blood, leading to the characteristic chest pain associated with angina.
Atherosclerosis involves the accumulation of cholesterol, fatty substances, cellular waste products, calcium, and fibrin on the inner walls of the arteries. These deposits, collectively referred to as plaques, can harden over time, causing the arteries to stiffen and narrow. This reduced arterial flexibility and narrowed passageway impede blood flow, effectively starving the heart muscle of the necessary oxygen and nutrients.
Beyond atherosclerosis, other causes of angina pectoris include coronary artery spasm, which is a temporary tightening of the muscles within the artery walls. This spasm can abruptly reduce or even cut off blood flow to the heart, similar to how traffic congestion on a busy highway can prevent cars from reaching their destination. Such spasms can occur in both healthy and atherosclerotic arteries and may be triggered by stress, exposure to cold, smoking, or the use of stimulant drugs like cocaine.
Severe anemia is another potential cause of angina pectoris. Anemia reduces the blood’s capacity to carry oxygen, effectively lowering the amount of oxygen available to the heart muscle. This condition can mimic the effects of reduced blood flow, resulting in angina-like symptoms.
Uncontrolled high blood pressure (hypertension) is also a significant contributor. Chronic hypertension forces the heart to work harder to pump blood, which can lead to thickening of the heart muscle (left ventricular hypertrophy) and increased oxygen demand. When this demand outstrips the supply due to narrowed or stiffened arteries, angina can occur.
Risk Factors of Angina Pectoris
Several factors can significantly increase the likelihood of developing angina pectoris. One of the most prominent risk factors is smoking. The harmful chemicals in tobacco can damage the heart and blood vessels, leading to the buildup of plaque and ultimately causing narrowed arteries. This increases the risk of angina and other cardiovascular diseases.
High blood pressure, or hypertension, is another critical risk factor. When blood pressure is consistently high, it forces the heart to work harder than normal, which can lead to the thickening of the heart muscle and narrowing of the arteries. This added strain can contribute to the onset of angina.
High cholesterol levels are also directly linked to an increased risk of angina pectoris. Cholesterol can accumulate in the arteries, forming plaques that narrow the passageways and restrict blood flow to the heart. Both low-density lipoprotein (LDL) cholesterol, known as “bad” cholesterol, and triglycerides can contribute to this buildup.
Diabetes is another significant risk factor. High blood sugar levels can damage blood vessels and the nerves that control the heart. People with diabetes often have other conditions that further increase their risk of angina, such as high blood pressure and high cholesterol.
Obesity and a sedentary lifestyle also play a substantial role in the development of angina. Excess weight can increase the strain on the heart, and lack of physical activity can contribute to the buildup of fatty deposits in the arteries. Engaging in regular physical activity and maintaining a healthy weight are crucial for reducing these risks.
Family history of heart disease is a non-modifiable risk factor. If your parents or close relatives had heart problems, you might be more likely to experience similar issues. This genetic predisposition can increase the risk of developing angina pectoris.
Other contributing factors include stress and unhealthy eating habits. Chronic stress can elevate blood pressure and lead to unhealthy behaviors such as overeating or smoking, further increasing the risk of angina. An unhealthy diet high in saturated fats, trans fats, and cholesterol can also contribute to the buildup of plaques in the arteries.
Remember the rhyme: “Smoke and stress, high BP mess, cholesterol’s high, risk is nigh.” By understanding and managing these risk factors, individuals can take proactive steps to reduce their chances of developing angina pectoris.
Complications of Angina Pectoris
If left untreated, angina pectoris can escalate into severe complications, significantly impacting one’s health. One of the most critical complications is a heart attack, or myocardial infarction. This occurs when the blood flow to a part of the heart is completely blocked, akin to a roadblock that halts all traffic, preventing oxygen and nutrients from reaching the heart muscle. This blockage can result in the death of heart tissue, presenting a life-threatening situation that requires immediate medical attention.
Another severe complication related to untreated angina pectoris is heart failure. In this condition, the heart loses its ability to pump blood efficiently throughout the body. Imagine the heart functioning as a pump; when it weakens, it cannot meet the body’s demands, leading to fatigue, shortness of breath, and fluid retention. Heart failure progressively worsens if not properly managed, further complicating the patient’s health profile.
Additionally, angina pectoris can lead to arrhythmias, which are irregular heartbeats. These can vary from harmless to life-threatening. The heart’s regular rhythm can be disrupted, causing it to beat too fast, too slow, or erratically. This disruption can impair the heart’s ability to pump blood effectively, potentially leading to fainting, stroke, or sudden cardiac arrest.
These complications of angina pectoris can set off a domino effect, where one issue precipitates another, creating a cascade of health problems. Therefore, timely diagnosis and effective management of angina are paramount in preventing these serious, potentially fatal outcomes. Maintaining regular medical check-ups, adhering to prescribed treatments, and making lifestyle modifications are essential steps to mitigate these risks and ensure better cardiovascular health.
Management of Angina Pectoris
Effective management of angina pectoris involves a multifaceted approach encompassing lifestyle adjustments, pharmacological intervention, and, in some cases, medical procedures. This comprehensive strategy aims to alleviate symptoms and reduce the risk of serious cardiovascular events.
The first step in managing angina pectoris is adopting healthy lifestyle changes. Smoking cessation is paramount, as tobacco use is a significant risk factor for angina and other cardiovascular diseases. A heart-healthy diet, rich in fruits, vegetables, whole grains, and lean proteins, can help improve overall cardiovascular health. Regular physical activity is also crucial; it improves heart function and helps maintain a healthy weight. Additionally, effective stress management practices, such as mindfulness and relaxation techniques, can help minimize angina episodes.
Medications play a vital role in the management of angina. Nitrates, such as nitroglycerin, are often prescribed to help dilate blood vessels and improve blood flow to the heart. Beta-blockers help reduce the heart’s workload by slowing the heart rate and lowering blood pressure. Calcium channel blockers can also be used to relax and widen blood vessels, enhancing blood flow. Collectively, these medications aim to alleviate angina symptoms and prevent future episodes.
In cases where lifestyle changes and medications are insufficient, medical procedures may be necessary. Angioplasty, a procedure that involves inflating a small balloon inside a narrowed artery to widen it, can restore adequate blood flow to the heart. Coronary artery bypass surgery, another option, involves creating a new pathway for blood to flow around a blocked artery. These interventions, although more invasive, can significantly improve the quality of life for individuals with severe angina.
The management of angina pectoris can be summarized using the mnemonic ‘SLIM’: Stop smoking, Lifestyle changes, Ingest medications, and Medical procedures. This multi-step approach ensures a comprehensive strategy to manage this condition effectively.