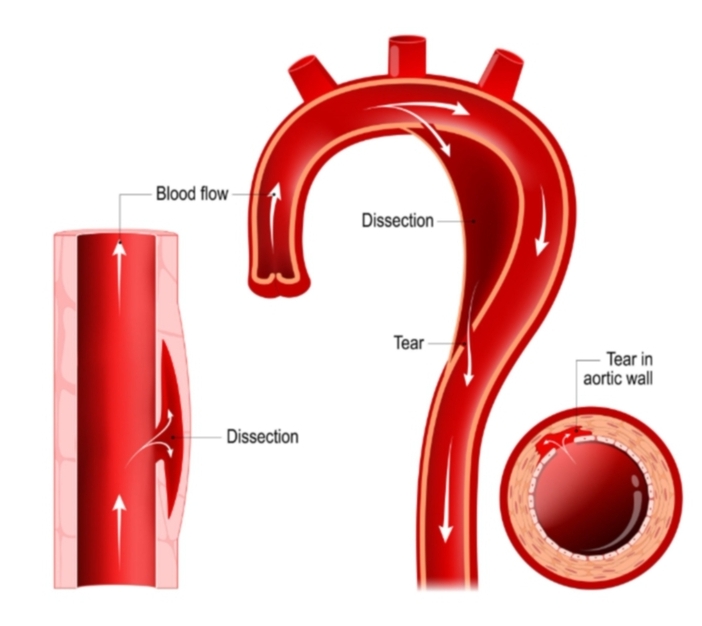
The aorta, a vital artery, plays a crucial role in our circulatory system by transporting oxygen-rich blood from the heart to the rest of the body. When discussing cardiovascular health, one condition that demands attention is aorta dissection. Aorta dissection occurs when there is a tear in the inner layer of the aorta’s wall. This tear allows blood to infiltrate between the layers of the aorta’s wall, causing the layers to separate. For better understanding, imagine a garden hose. If the inner lining of the hose were to tear, water would start to stream between the layers of the hose, causing them to divide and weaken. Similarly, an aorta dissection can be detrimental and poses significant health risks. Proper awareness and timely medical intervention are crucial in managing this condition effectively.
Real-Life Scenario
John, a 52-year-old man with a history of high blood pressure, woke up one morning with a strange sensation in his chest. The discomfort quickly escalated into severe, excruciating pain that felt like something was tearing inside him. Alarmed, John clutched his chest, feeling the intense pain radiate to his back and down his legs.
Recognizing that something was seriously wrong, John’s wife called emergency services immediately. As the paramedics arrived and assessed his condition, John’s symptoms included dizziness, shortness of breath, and a feeling of impending doom. The paramedics acted quickly, rushing him to the nearest hospital.
At the emergency room, the doctors conducted a series of diagnostic tests, including a CT scan, which confirmed their suspicions of an aortic dissection. This condition occurs when the inner layer of the aorta, the large blood vessel branching off the heart, tears. Blood surges through the tear, separating the layers of the aortic wall, creating a false lumen. Aortic dissection is a medical emergency requiring prompt diagnosis and intervention to prevent catastrophic complications, including rupture or obstruction of critical blood vessels.
The cardiovascular team informed John about the gravity of his condition, explaining that immediate surgery was necessary to repair the dissection and prevent further damage. The surgery involved replacing the damaged portion of the aorta with a synthetic graft. Knowing the urgency, John consented to the procedure, aware that swift action was essential for his survival.
Fortunately, the surgery was successful, and John was transferred to the intensive care unit for close monitoring. Over the following weeks, he slowly recovered, learning the importance of managing his blood pressure and attending regular follow-ups to prevent recurrence. John’s experience underscores the critical nature of recognizing symptoms early and seeking immediate medical attention in cases of suspected aortic dissection.
Understanding the Symptoms
Aorta dissection can be a serious condition, and recognizing its symptoms early is crucial. To help remember the signs, think of this simple rhyme: “Hey, sudden pain, sharp as rain, back and belly feel the strain.” This easy mnemonic can be a lifesaver when understanding the indicators of an aortic dissection. Here are some common symptoms to be aware of:
Sudden Chest Pain: One of the hallmark symptoms is sudden, severe chest pain. It is often described as a tearing or ripping sensation that can extend to the back. This pain can be extremely intense and may feel different from a heart attack.
Back Pain: Alongside chest pain, many individuals report a sharp pain in the upper back. This pain is often a result of the dissection spreading along the aorta and can extend down into the lower back as well.
Belly Pain: Discomfort in the abdomen is another possible symptom. The pain can be severe and may feel like a deep ache or sharp stabbing sensation.
Fainting: Sudden fainting or a feeling of lightheadedness can occur due to a decrease in blood flow. Fainting is a serious sign and requires immediate medical attention.
Shortness of Breath: Difficulty breathing or shortness of breath can accompany other symptoms. This can be due to the heart struggling to pump blood efficiently or fluid building up in the lungs.
It’s important to note that symptoms can vary widely from person to person. Some may experience all these signs, while others might only suffer from a few. Additionally, the intensity of the symptoms can differ, making it essential to seek medical advice if any signs are present. Recognizing these symptoms promptly can make a significant difference in the treatment and outcome of aortic dissection.
Who is at Risk?
Understanding the risk factors for aorta dissection is essential for early detection and prevention. To better grasp these risks, remember this simple rhyme: “High pressure, weak tissues, surgery issues.” Let’s delve into each part to see how they contribute to the likelihood of experiencing an aorta dissection.
Firstly, “high pressure” refers to high blood pressure, also known as hypertension. When the force of the blood against the walls of your arteries is consistently too high, it puts extra stress on the heart and blood vessels. Imagine blowing too much air into a balloon; eventually, its walls could weaken or even tear. In the same way, persistently high blood pressure can wear down the aorta, the body’s main artery, leading to an increased risk of dissection.
Next, “weak tissues” points to connective tissue disorders. Conditions such as Marfan syndrome and Ehlers-Danlos syndrome affect the strength and elasticity of the connective tissues in the body. In individuals with these disorders, the aorta can be more fragile and susceptible to tearing or rupturing. Picture a rope that has been frayed; under stress, it is more likely to break. Likewise, weak connective tissues can make the aorta more prone to dissection.
Lastly, “surgery issues” covers individuals who have undergone previous heart surgeries. Surgical procedures, particularly those involving the heart and aorta, can leave scars or areas of weakness in the aortic wall. These weakened spots can become points of vulnerability, especially under physical stress. It can be akin to patching a worn-out tire; while it might hold, it’s more susceptible to damage than an unblemished one.
By understanding these key risk elements—high blood pressure, connective tissue disorders, and a history of heart surgeries—we can better anticipate and manage the chances of aorta dissection. Remembering “high pressure, weak tissues, surgery issues” helps to keep these risks in mind, ensuring vigilance and proactive health management.
Diagnosis Made Easy
In diagnosing aortic dissection, medical professionals employ a range of technologies to ensure accurate and timely identification. One of the primary methods used is the CT scan, which can be likened to a high-resolution camera capturing detailed images of the body’s internal structures. Just as a photographer adjusts the focus to get a clearer image, the CT scan takes cross-sectional pictures of the aorta, allowing doctors to identify any tears or abnormalities.
Another crucial diagnostic tool is the MRI, or Magnetic Resonance Imaging. Picture an MRI as a sophisticated scanner that uses magnets and radio waves to create detailed images of the heart and blood vessels. This method is particularly valuable because it can provide a comprehensive view without the need for radiation, making it a safer option for certain patients.
Ultrasounds also play a pivotal role in diagnosing aortic dissection. They function similarly to sonar used by submarines, sending sound waves into the body and translating the echoes into visual images. This method, known as an echocardiogram when focused on the heart, is especially beneficial for real-time assessments and can reveal abnormalities in the aorta’s structure and function.
In some cases, doctors might also use an angiogram, a special type of X-ray that involves injecting a contrast dye into the bloodstream. This dye makes the blood vessels visible on the X-ray images, helping to highlight areas where the dissection may be occurring. Think of it as adding color to a black and white drawing, making it easier to detect and diagnose issues.
Merging these tests provides a comprehensive picture, much like assembling pieces of a jigsaw puzzle to form a complete image. Early and accurate diagnosis of aortic dissection is critical, as it significantly influences the treatment plan and ultimately, patient outcomes.
Treatment Options
Aorta dissection requires prompt and precise treatment to prevent severe complications. The treatment approach can be broadly classified into surgical and non-surgical options, akin to repairing a torn hose versus managing the water pressure through adjustments.
Surgical treatment involves repairing or replacing the damaged section of the aorta, much like fixing a tear in a hose to prevent water from leaking. This procedure, often known as aortic repair, can be conducted through open surgery or endovascular techniques. In open surgery, a surgeon makes an incision in the chest to directly access and repair the aorta. Endovascular procedures are less invasive, involving a catheter inserted through the groin to place a stent graft, which reinforces the weakened section.
On the other hand, non-surgical treatment aims at managing the condition using medications and lifestyle adjustments, similar to controlling the water pressure in a system rather than fixing the tear. Medications such as antihypertensives help in reducing the blood pressure and heart rate, minimizing stress on the aorta and potentially halting the progression of the dissection. Beta-blockers, calcium channel blockers, and angiotensin-converting enzyme (ACE) inhibitors are commonly prescribed for this purpose.
Regardless of the treatment path, timely intervention is critical for a favorable outcome. Delays in addressing aorta dissection can lead to life-threatening complications such as rupture or severe internal bleeding. Therefore, swift diagnosis followed by an appropriate treatment plan, tailored to the patient’s specific condition and health status, is essential.
In conclusion, a balanced approach combining surgical and non-surgical methods, under the guidance of a medical professional, serves as the cornerstone for managing aorta dissection efficiently. This two-fold strategy, targeting both repairing the structural damage and optimizing the physiological parameters, underscores the intricacies involved in treating this critical condition.
Living with Aorta Dissection
Experiencing an aortic dissection is undoubtedly life-altering; however, with diligent care and appropriate adjustments, individuals can continue to lead fulfilling lives. One of the most crucial aspects of managing life post-diagnosis is understanding the importance of lifestyle changes. Regular monitoring and maintaining stable blood pressure becomes a cornerstone of daily routine. High blood pressure is a significant risk factor for further complications, so it’s essential to follow a prescribed medication regimen and make necessary dietary changes.
Maintaining a heart-healthy diet is critically important for those living with aortic dissection. Focus on consuming heart-friendly foods, rich in fruits, vegetables, whole grains, and lean proteins. Reducing salt intake can help keep blood pressure in check, and avoiding processed foods and excess sugars can contribute to overall cardiovascular health. Regular physical activity, as recommended by healthcare providers, plays an equally vital role. Gentle exercises, such as walking or swimming, can improve cardiovascular health without putting undue strain on the body.
In addition to lifestyle modifications, consistent medical follow-ups are imperative. Regular check-ups aid in monitoring the condition of the aorta and ensure that any changes are detected early. Healthcare professionals might recommend periodic imaging tests, such as CT scans or MRIs, to monitor the dissection and respond promptly if any issues arise. Keeping an open line of communication with healthcare providers helps in adjusting treatment plans and incorporating any new medical advances or findings.
It’s also beneficial for individuals to engage emotionally and psychologically by seeking support from family, friends, or support groups. These networks can provide encouragement and advice, making the journey less isolating. By integrating these practical steps into daily life, those with aortic dissection can significantly improve their quality of life and manage their condition more effectively.
Conclusion and Key Takeaways
Aorta dissection is a serious and potentially life-threatening condition that requires immediate medical attention. By understanding the risk factors, symptoms, and treatment options, individuals can significantly improve their chances of successful outcomes. It’s vital to recognize the warning signs, such as sudden, severe chest pain that may spread to the back or abdomen, along with accompanying symptoms like shortness of breath, fainting, or a rapid pulse.
The importance of seeking immediate medical assistance cannot be overstated. Diagnosing aorta dissection promptly through imaging tests such as CT scans, MRIs, or echocardiograms is crucial for determining the appropriate treatment pathway, which may range from medication management to emergency surgery.
Individuals at higher risk, including those with a family history of the condition, hypertension, or connective tissue disorders, should maintain regular check-ups and communicate any unusual symptoms to their healthcare provider. Preventive measures such as managing blood pressure, avoiding smoking, and adhering to a heart-healthy lifestyle also play a key role in mitigating the risk of aorta dissection.
In conclusion, awareness and swift action are the cornerstones of managing aorta dissection, underscoring the critical need for early detection and timely intervention. Remember, proper medical guidance and proactive health practices can make this serious condition more manageable.
When the aorta’s in trouble,
Don’t wait, double the haste,
And see the doctor face to face.


