Introduction to Aortitis
Aortitis, in its simplest terms, refers to the inflammation of the aorta, which is the body’s main artery responsible for transporting oxygenated blood from the heart to various organs. To visualize this, imagine the aorta as a garden hose. Just as a garden hose delivers water to plants in your garden, the aorta delivers blood to organs throughout your body. If your garden hose develops a blockage or kink, the flow of water is disrupted, affecting the health of your plants. Similarly, when the aorta becomes inflamed, it can hamper the blood flow and jeopardize the health of various organs.
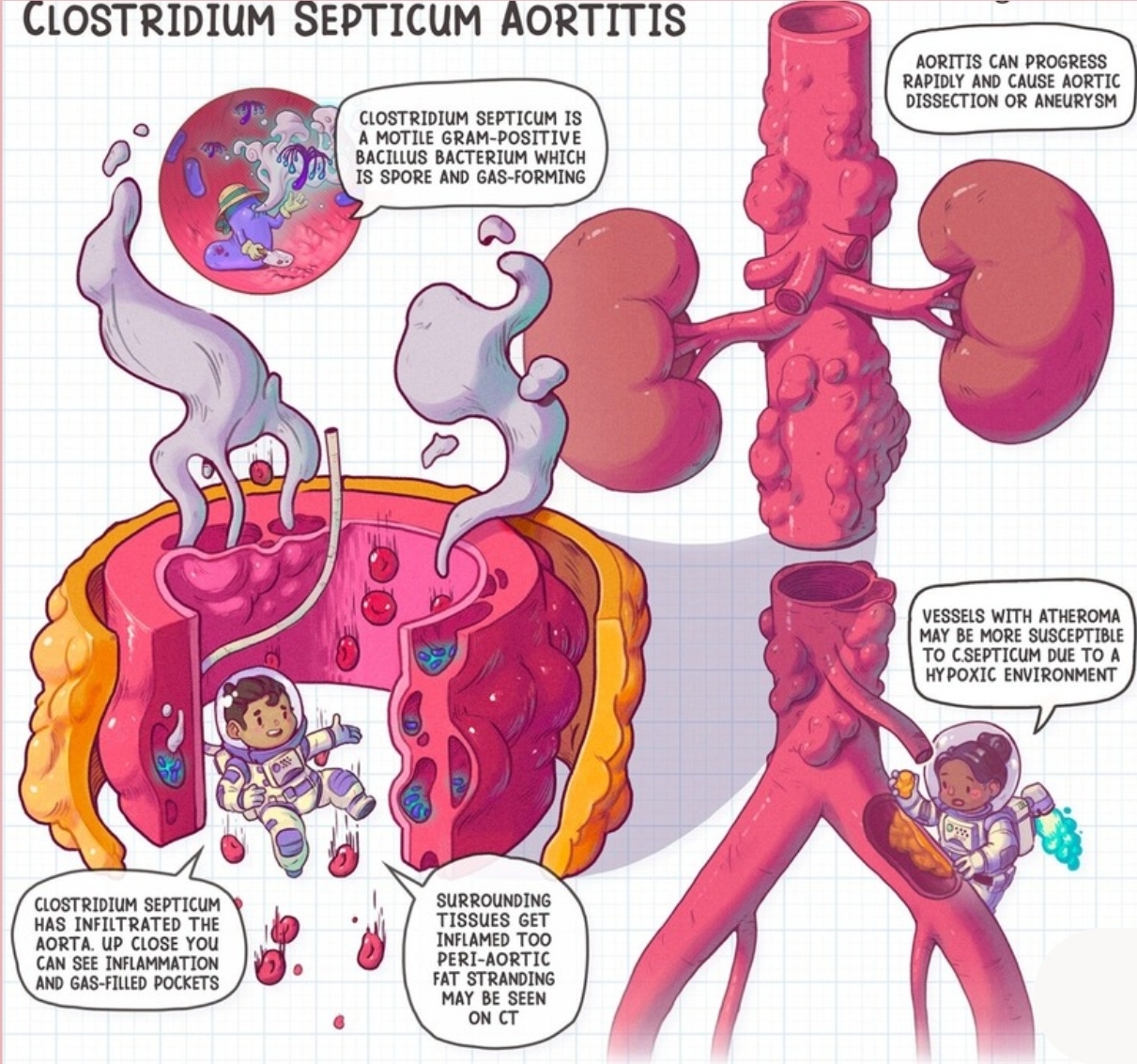
This inflammation could be triggered by a variety of factors, including infections, autoimmune conditions, or other underlying diseases. When the aorta is inflamed, it can lead to a range of serious conditions such as aneurysms (abnormal bulging of the artery) or dissections (tears in the artery wall). Both of these complications can have life-threatening consequences if not promptly diagnosed and treated.
The symptoms of aortitis can be nonspecific, often mimicking those of other medical conditions, which makes it challenging to diagnose. Symptoms might include chronic fatigue, fever, chest or back pain, and even reduced pulses in the extremities. Due to these vague symptoms, it’s crucial for medical professionals to consider aortitis in their differential diagnosis when patients present with unexplained systemic symptoms.
Recognizing aortitis early is pivotal for preventing its progression to severe or fatal outcomes. Medical imaging and a thorough clinical evaluation are essential tools for diagnosing this condition. Understanding the basic concept of aortitis and its potential impact on the body prepares individuals to appreciate the importance of prompt medical evaluation and treatment.
Real-Life Scenario: Emily’s Experience
Emily, a 32-year-old professional, initially attributed her persistent fatigue to the demands of her hectic lifestyle. However, when coupled with an unexplained fever, she began to suspect that something more serious might be affecting her health. Driving home from work one evening, Emily experienced an alarming bout of chest pain, prompting her to seek medical attention immediately.
Emily’s journey to diagnosis began with her first visit to the local clinic, where the doctor ordered preliminary blood tests and an electrocardiogram (ECG) to rule out common heart conditions. Despite normal test results, Emily’s symptoms persisted. Unconvinced by the initial findings and concerned about her health, her primary care physician referred her to a cardiologist for further evaluation.
At the cardiologist’s office, a more thorough exam included advanced imaging techniques such as a computed tomography (CT) scan and magnetic resonance imaging (MRI) of her chest. These tests revealed inflammation in the wall of the aorta, a major artery of the heart, leading the cardiologist to suspect aortitis. Her symptoms were beginning to make sense, but a definitive diagnosis still required additional testing.
Emily’s diagnosis of aortitis was confirmed after a biopsy and a series of laboratory tests targeting specific markers of inflammation. Her healthcare team explained that aortitis is a rare condition characterized by inflammation of the aorta, which can lead to serious complications if left untreated. Finally understanding what was causing her symptoms, Emily began a treatment plan that included anti-inflammatory medications and regular follow-up visits to monitor her condition.
Managing aortitis has significantly impacted Emily’s daily life, requiring her to be vigilant about her health and maintain a close relationship with her healthcare providers. Through lifestyle adjustments and ongoing treatment, she aims to manage her condition effectively, while staying informed about potential flare-ups and complications. Emily’s experience underscores the importance of persistence in seeking a diagnosis and the critical role of specialized care in managing rare medical conditions like aortitis.
Symptoms and Signs
Aortitis, an inflammation of the aorta, manifests through a variety of symptoms that can greatly affect an individual’s quality of life. Recognizing these symptoms early on is crucial in managing and treating the condition effectively. A practical mnemonic to remember the symptoms of aortitis is ‘F-F-C-W-C-D,’ representing Fatigue, Fever, Chest pain, Weight loss, Chest tightness, and Difficulty breathing.
Fatigue: Individuals with aortitis often experience persistent fatigue, making even routine tasks exhausting. This is due to the systemic inflammation that drains the body’s energy. For instance, someone may find themselves unusually tired after a short walk or light household chores.
Fever: A recurring or continuous fever may be a sign of aortitis. The body’s response to inflammation often includes an elevated temperature. For example, a person might notice they consistently feel warmer than usual without any apparent cause like an infection or common cold.
Chest Pain: Chest pain is a significant indicator of aortitis. It can be sharp or dull and may radiate towards the back or abdomen. A person might experience sudden, intense chest pain while at rest or during physical activity, prompting immediate concern for their cardiovascular health.
Weight Loss: Unintended weight loss is another symptom of aortitis. This can occur due to the body’s increased metabolic demands fighting the inflammatory process. For example, someone may observe a noticeable drop in their weight over a few weeks without changes in diet or exercise routines.
Chest Tightness: Individuals might feel an uncomfortable tightness in their chest, akin to a squeezing sensation. This symptom can make breathing and daily activities challenging, often exacerbating existing fatigue and discomfort.
Difficulty Breathing: Breathing difficulties or shortness of breath are common in aortitis patients. This can occur due to the inflammation affecting the aorta’s function, leading to reduced oxygen delivery. A person may feel winded after climbing a flight of stairs or even while speaking, indicating a need for medical evaluation.
Understanding these symptoms helps in early detection and management of aortitis, but any unusual or persistent symptoms should always be discussed with a healthcare provider for accurate diagnosis and treatment.
Causes and Risk Factors
Aortitis, an inflammation of the aorta, can be triggered by various causes. Understanding these underlying causes is crucial for effective diagnosis and treatment. The mnemonic ‘INTACT’ provides a helpful way to remember the main categories of causes: Infection, Non-infectious, Trauma, Autoimmune, Chemical, and Tissue disorders.
Infection (I): Various infections can lead to aortitis. Bacterial infections, including syphilis and tuberculosis, are notable culprits. These pathogens can invade the walls of the aorta, leading to inflammation. Additionally, fungal infections like aspergillosis and viral infections such as HIV are also risk factors.
Non-infectious (N): Certain non-infectious conditions, such as chronic inflammatory diseases, can also cause aortitis. For example, severe atherosclerosis, which involves the buildup of plaques within the arterial walls, can result in inflammation and subsequent damage to the aorta.
Trauma (T): Physical trauma to the aorta, such as from a car accident or a high-impact injury, can precipitate aortitis. The damage to the aortic wall can incite inflammation as the body attempts to heal the affected area.
Autoimmune (A): Autoimmune disorders play a significant role in the development of aortitis. Conditions like giant cell arteritis and Takayasu arteritis are prime examples where the immune system mistakenly attacks the aorta, causing inflammation and damage. These diseases require prompt attention and treatment to prevent severe complications.
Chemical (C): Exposure to certain chemicals or drugs can provoke an inflammatory response within the aorta. For instance, some medications, especially certain chemotherapeutic agents, can have inflammatory side effects that impact the vascular system.
Tissue disorders (T): Genetic and connective tissue disorders such as Marfan syndrome and Ehlers-Danlos syndrome also increase the risk of aortitis. These conditions affect the structure and integrity of the aortic wall, making it more susceptible to inflammation and other complications.
By understanding the diverse causes encapsulated by the mnemonic ‘INTACT’, healthcare providers can better diagnose and manage aortitis, tailoring interventions to the underlying cause and improving patient outcomes.
Diagnosis: The Detective Work
Diagnosing aortitis can be likened to the intricate work of a detective piecing together a puzzle. Physicians rely on a combination of techniques to track down the precise cause and extent of the inflammation in the aorta. This meticulous process begins with a detailed physical examination, often prompting further investigation through blood tests and advanced imaging techniques.
The initial physical examination serves as the first layer of clues. Physicians look for signs such as a new heart murmur, high blood pressure differences between limbs, or unusual sounds from blood flow. These findings alone hint at potential underlying issues with the aorta but aren’t conclusive. They primarily guide the direction of the subsequent ‘detective’ work.
Next come blood tests, which are crucial in the diagnostic journey. In cases of aortitis, certain markers of inflammation, like elevated levels of C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR), may be found. These results add another piece to the puzzle, suggesting an inflammatory process occurring within the body. Furthermore, blood cultures might be performed if an infectious cause is suspected. Each clue garnered from these tests narrows down the potential culprits behind the condition.
Advanced imaging techniques, including computed tomography (CT) scans, magnetic resonance imaging (MRI) scans, and positron emission tomography (PET) scans, are often the final and most revealing steps in diagnosing aortitis. CT and MRI scans provide detailed images of the aorta, allowing physicians to visualize any changes or thickening of the arterial wall. These images can highlight the degree and location of inflammation, helping to map the extent of the disease accurately. A PET scan can identify metabolic activity in the tissues, which is particularly useful in detecting inflammatory changes.
Each diagnostic tool adds another layer to understanding the condition, much like pieces of a jigsaw puzzle coming together. Through this methodical approach, physicians can diagnose aortitis accurately, providing a solid foundation for crafting an effective treatment plan.
Treatment and Management
Aortitis, an inflammation of the aorta, can be a daunting condition, yet effective treatment options are available to manage and potentially alleviate its symptoms. As a general approach, a combination of medication and occasionally surgery forms the crux of aortitis management. With a little rhyme – “Pills and drills to save you still” – we can simplify these complex treatment modalities.
Medication is often the first line of defense. Corticosteroids, commonly known as steroids, play a pivotal role in reducing inflammation. These powerful anti-inflammatory agents are essential in controlling the immune system’s hyperactive response, which is a hallmark of aortitis. Alongside steroids, immunosuppressants may also be prescribed to prevent further immune system attacks on the aorta. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) are sometimes employed to manage associated pain and inflammation. In cases where infection is the underlying cause, antibiotics are crucial.
Surgery is reserved for specific scenarios where complications like aneurysms or significant aortic damage arise. Surgical interventions might involve the repair or replacement of affected portions of the aorta, ensuring uninterrupted blood flow and reducing the risk of life-threatening consequences. These “drills” in the rhyme refer to the precision and skill required in the surgical procedure.
However, treatment and management of aortitis don’t end with pills and surgery. Lifestyle modifications are integral to holistic care. Adopting a heart-healthy diet, engaging in regular physical activity, and managing stress can significantly impact overall well-being and long-term outcomes. Patients are encouraged to avoid smoking and limit alcohol consumption, as these habits can exacerbate cardiovascular issues.
Regular follow-ups with healthcare providers are crucial in monitoring the condition and making necessary adjustments to the treatment plan. These check-ups help in detecting any early signs of complications, ensuring timely interventions.
Thus, with a balanced approach that includes medication, potential surgical intervention, lifestyle alterations, and diligent medical oversight, effective management of aortitis can indeed be achieved.
Prognosis and Living with Aortitis
The long-term outlook for individuals diagnosed with aortitis can vary significantly depending on the severity of the condition and how promptly it is managed. While facing aortic inflammation might initially seem daunting, it is crucial to maintain a positive yet realistic perspective. With proper treatment and lifestyle adjustments, many individuals diagnosed with aortitis can lead fulfilling lives.
Consider the story of Emily. Diagnosed with aortitis at the age of 34, she initially experienced a surge of anxiety about her future. However, once she commenced her treatment plan—which included medication to manage inflammation and regular check-ups to monitor her condition—she began to see improvements in her health. Emily also made lifestyle adjustments, such as incorporating a heart-healthy diet and moderate exercise into her routine, which helped enhance her overall well-being.
Emily’s story underscores the importance of medical adherence and lifestyle modifications. Individuals with aortitis should work closely with their healthcare providers to develop a personalized treatment plan. This may involve immunosuppressive or corticosteroid therapy to reduce inflammation, as well as routine imaging tests to monitor the aorta’s condition. By following their prescribed treatment regimen meticulously, patients can prevent complications and improve their quality of life.
In addition to medical treatment, support systems play a vital role in living with aortitis. Emily found solace and motivation in support groups, where she connected with others facing similar health challenges. Building a strong network of friends, family, and healthcare professionals can provide emotional support, practical advice, and encouragement.
While aortitis may bring challenges, it is evident from Emily’s experience and those of others living with this condition that a proactive, informed approach can lead to a meaningful life. With the right tools and mindset, patients can thrive, navigating their journey with resilience and optimism.
Preventive Measures and Final Thoughts
Maintaining a healthy lifestyle plays a crucial role in reducing the risk of aortitis. Adopting balanced nutrition and engaging in regular physical activity can significantly enhance one’s overall cardiovascular health. Consuming a diet rich in fruits, vegetables, lean proteins, and whole grains while limiting saturated fats, sugar, and salt, helps in maintaining optimal blood pressure and cholesterol levels—key factors in preventing inflammation of the aorta.
Addressing infections promptly and effectively is another essential preventive measure. It is important to follow through with prescribed treatments for bacterial and viral infections to prevent complications that may lead to aortitis. Regular medical check-ups enable early detection and timely intervention, thus forestalling potential progression to more severe forms of the condition. Ensuring up-to-date vaccinations can also safeguard against infectious agents that might contribute to the development of aortitis.
Additionally, managing pre-existing health conditions, such as autoimmune diseases, that can predispose individuals to aortitis is vital. This involves consistent monitoring and communication with healthcare providers to keep these conditions under control and reduce risks. Adhering to prescribed medication regimens and maintaining a clear and cooperative relationship with healthcare professionals can offer substantial benefits.
While aortitis can be a daunting prospect, increased awareness and a proactive approach to health management can significantly mitigate its impact. Staying informed about potential symptoms, seeking medical advice when necessary, and adhering to recommended lifestyle modifications can empower individuals to take control of their cardiovascular health effectively.
Ultimately, the vigilance in preventive health measures can help manage the risk of aortitis, fostering a sense of confidence and resilience. By prioritizing healthy living, individuals can bolster their defenses against this condition, ensuring a better quality of life. Through consistent effort and informed choices, the journey toward optimal cardiovascular health remains within reach.