Introduction to Peptic Ulcers
Peptic ulcers are open sores that form on the inner lining of your stomach, lower esophagus, or small intestine. These sores occur when the thick layer of mucus that protects your digestive tract from stomach acid diminishes, allowing the acid to erode the tissue on the linings of the aforementioned organs. Imagine having a paper cut on your hand; now think of that cut inside your stomach or small intestine where digestive juices continually bombard the damaged area. This scenario gives you a sense of the pain and discomfort individuals with peptic ulcers experience.
If you’ve ever felt a burning or gnawing pain in your stomach, especially between meals or at night, you might be familiar with one of the common symptoms of peptic ulcers. These ulcers don’t just disrupt your digestive system; they can also significantly impact your day-to-day well-being. Consider how frustrating it can be when your stomach feels like it’s on fire just as you’re sitting down for a family meal. Or think about the irritation of waking up in the middle of the night because of persistent discomfort.
Understanding the nature of peptic ulcers is crucial for managing them effectively. When untreated, these ulcers can lead to more serious complications, such as bleeding, perforation, or gastrointestinal obstruction. Therefore, recognizing their presence early on, understanding their causes, and knowing when to seek medical advice can prevent deterioration and foster better health outcomes.
By setting the foundation with a clear and straightforward explanation, we aim to demystify peptic ulcers. In the sections that follow, we will dive deeper into the various aspects of this condition, including its causes, symptoms, and available management strategies. This comprehensive overview will equip you with the knowledge needed to better understand and address peptic ulcers, either for yourself or for someone you care about.
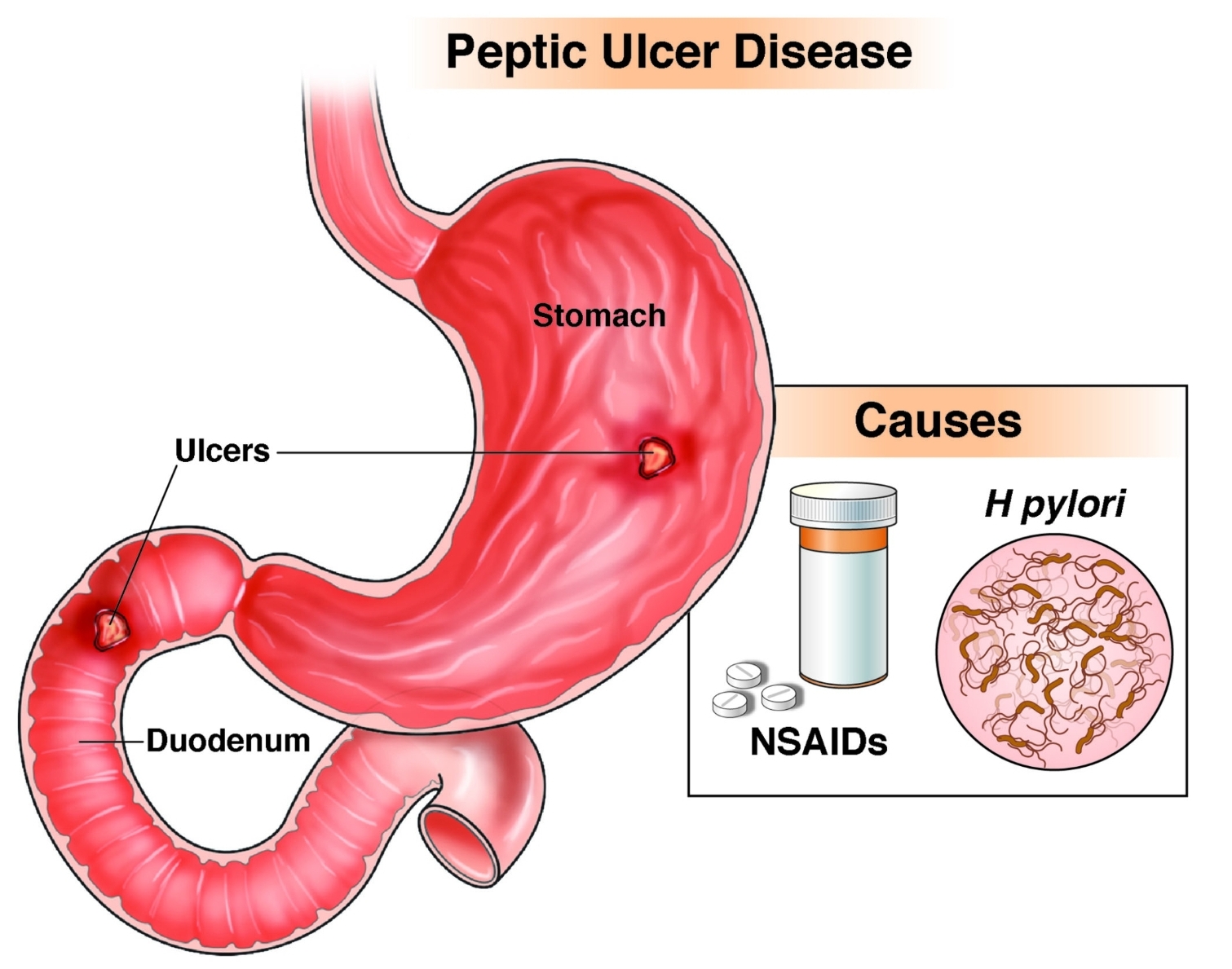
Causes of Peptic Ulcers
Peptic ulcers are primarily caused by an imbalance between the digestive fluids in the stomach and duodenum, largely influenced by certain harmful factors. One of the most common culprits behind the development of peptic ulcers is the Helicobacter pylori (H. pylori) bacteria. This bacterium, residing in the mucous layer of the stomach, can cause inflammation and weaken the stomach’s defenses against the acidic environment, ultimately leading to ulcer formation. Many people infected with H. pylori may not exhibit symptoms immediately, but over time, the persistent bacterial infection can result in the development of ulcers.
An additional significant factor in the occurrence of peptic ulcers is the prolonged use of nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and aspirin. These medications can impair the stomach’s ability to produce the protective mucus necessary to prevent damage by stomach acid. Without this protective layer, the stomach lining becomes more susceptible to ulcers. Individuals who regularly consume NSAIDs for chronic pain management or other medical conditions are at a heightened risk of developing peptic ulcers.
Stress and diet also play roles, albeit secondary, in contributing to peptic ulcer etiology. While it was once widely believed that stress was a major cause of ulcers, current medical understanding underscores that stress exacerbates existing conditions rather than directly causing them. For instance, an individual experiencing substantial stress may have increased gastric acid production, which can worsen a pre-existing ulcer. Moreover, certain dietary habits, such as consuming spicy foods, coffee, and alcohol, might not directly cause ulcers but can irritate the stomach lining and aggravate existing conditions.
Consider the scenario of a middle-aged individual who juggles a high-stress job and relies on NSAIDs to manage chronic headaches. Over time, the combined impact of stress-induced gastric acidity and the compromised protective mucus layer from NSAID overuse can culminate in the development of a painful peptic ulcer. Understanding the causative factors of peptic ulcers enables better prevention and management strategies, ensuring more effective care for those affected.
Symptoms and Signs of Peptic Ulcers
Understanding the symptoms and signs of peptic ulcers is crucial for early detection and prompt management. One of the most common symptoms is a burning stomach pain. This pain typically occurs between meals and in the middle of the night when the stomach is empty. It’s usually exacerbated by hunger and can temporarily subside upon eating food or taking antacids, only to return later. This cyclical nature is a hallmark feature of peptic ulcer pain.
Bloating is another frequent symptom associated with peptic ulcers. Individuals often describe a sensation of fullness or swelling in the abdomen, which might be consistent or recurrent. Heartburn, which is a burning sensation in the chest, can also accompany peptic ulcers. This is especially true if the ulcer is located in the upper section of the stomach or the beginning of the small intestine.
Nausea and, occasionally, vomiting can be additional indicators. The nausea may not be severe but tends to be persistent and can significantly impact a person’s quality of life. In some cases, the presence of a more severe underlying condition may be indicated if vomiting continues or if there is blood in the vomit, which appears red or has a coffee ground-like texture.
To better illustrate these signs, consider the experience of an office worker who notices that their stomach pain intensifies after skipping breakfast and seems to better after lunch. This individual may also find themselves unable to enjoy meals due to persistent bloating and a recurring bout of heartburn that flares up after consuming certain foods. Additionally, there might be episodes of mild nausea that disrupt daily routines, causing discomfort and concern.
Correctly identifying these symptoms in oneself or others can be pivotal in diagnosing peptic ulcers early, allowing for timely medical intervention and improved management. If you recognize these symptoms persistently appearing in day-to-day activities, consulting a healthcare provider is advised.
Complications of Peptic Ulcers
Peptic ulcers, when left untreated, can lead to a range of severe complications that significantly impact an individual’s health and quality of life. One of the most common complications is bleeding. Gastrointestinal bleeding from an ulcer can present as vomiting blood or passing black, tarry stools. Such bleeding can lead to anemia, characterized by fatigue, weakness, and pallor. In extreme cases, significant blood loss may require hospital admission and blood transfusions.
Another critical complication is perforation. Perforation occurs when an ulcer eats through the wall of the stomach or duodenum, creating an open hole. This condition results in the contents of the stomach or intestines leaking into the abdominal cavity, causing severe pain and peritonitis – a potentially life-threatening inflammation of the peritoneum. Perforation is an emergency that requires immediate surgical intervention.
Gastric obstruction is also a potential issue, particularly when an ulcer swells, scars, or causes chronic inflammation, leading to a blockage in the digestive tract. Individuals with gastric obstruction might experience recurrent vomiting, feeling full after eating only small amounts of food, and weight loss. This condition necessitates prompt medical evaluation and treatment to prevent malnutrition and further complications.
Real-life scenarios underscore the importance of early intervention. For instance, an individual who ignores recurring ulcer symptoms might find themselves in urgent care with severe gastrointestinal bleeding that could have been addressed earlier with medications or lifestyle changes. Another scenario involves a patient experiencing sudden, sharp abdominal pain due to perforation, requiring emergency surgery that could have been avoided with timely ulcer treatment.
These complications highlight the urgent need for individuals with symptoms of peptic ulcers to seek medical advice promptly. Early diagnosis and appropriate treatment can prevent these potentially life-threatening conditions and ensure better health outcomes. Therefore, recognizing the seriousness of peptic ulcers and taking early action cannot be overemphasized.
Pathophysiology of Peptic Ulcers
Peptic ulcers result from a complex interplay of various biological and physiological processes. At the core of ulcer formation are three primary factors: acid production, mucosal defense mechanisms, and bacterial infection, particularly Helicobacter pylori.
To understand how these factors contribute to ulcer development, imagine the stomach as a high-security facility. The stomach lining (mucosa) serves as the fortress walls, protecting against the corrosive effects of gastric acid, much like strong stone walls ward off invaders. The body secretes mucus, which forms a gel-like protective barrier over the mucosa, similar to how a moat safeguards a castle.
However, this delicate balance can be disrupted. Gastric acid, which aids in food digestion, is like the facility’s armed guards—not harmful when kept in check but dangerous if unregulated. Factors such as stress, spicy food, and certain medications like NSAIDs (non-steroidal anti-inflammatory drugs) can stimulate excess acid production, akin to the guards turning rogue. Excess acid can erode the mucus layer and attack the stomach lining.
Another critical element in peptic ulcer pathophysiology is the presence of Helicobacter pylori. This bacterium is like a cunning infiltrator that can breach the fortress walls. Helicobacter pylori weakens the mucus barrier, making it easier for gastric acid to cause damage. It also triggers an inflammatory response, compounding the injury to the stomach’s protective lining.
While excess acid and Helicobacter pylori are key players, compromised mucosal defenses also contribute significantly. Normally, this lining has restorative mechanisms, including rapid cell turnover and adequate blood flow, which facilitate quick healing. However, if these defenses are impaired—due to aging, smoking, or chronic use of certain medications—the repair process falters, and the risk of ulcers increases.
In conclusion, peptic ulcers stem from an imbalance between aggressive factors like excess acid and Helicobacter pylori and the stomach’s defensive mechanisms. Understanding these biological interactions can help in comprehending the development and treatment of peptic ulcers effectively.
Management and Treatment of Peptic Ulcers
The management and treatment of peptic ulcers involves a multifaceted approach that aims not only to alleviate symptoms but also to promote healing and prevent recurrence. The primary strategies include medication, lifestyle adjustments, and in severe cases, surgical intervention. When collectively employed, these methods can contribute to effective ulcer management and significantly enhance the quality of life for affected individuals.
Medications often constitute the first line of treatment for peptic ulcers. Proton pump inhibitors (PPIs) such as omeprazole and lansoprazole are commonly prescribed to reduce gastric acid production, thereby minimizing irritation of the ulcerated area and facilitating the healing process. In cases where infection by the bacterium Helicobacter pylori is identified, a regimen of antibiotics is administered alongside PPIs to eradicate the bacteria. This dual approach not only addresses the immediate symptoms but also tackles the underlying cause, thus reducing the risk of recurrence.
Lifestyle changes play a crucial role in managing peptic ulcers. Patients are advised to avoid foods and beverages that can exacerbate symptoms, such as spicy foods, alcohol, and caffeine. Smoking cessation is also highly recommended, as tobacco use has been linked to delayed ulcer healing and increased recurrence rates. Stress management techniques, including mindfulness meditation and regular physical activity, can further aid in reducing symptom severity and improving overall wellness.
In situations where peptic ulcers do not respond to medication or lead to complications such as severe bleeding, surgical interventions may be considered. Procedures such as vagotomy, which involves cutting nerves to reduce acid secretion, or gastrectomy, the partial removal of the stomach, can be effective in treating persistent or complicated ulcers. These options, though more invasive, can provide long-term relief and prevent serious health issues stemming from untreated peptic ulcers.
Real-life scenarios attest to the efficacy of these management strategies. For instance, a patient with a persistent ulcer who adhered to a regimented PPI and antibiotic treatment, coupled with dietary modifications and smoking cessation, experienced significant symptom relief and successful ulcer healing. Another case involved a patient with a bleeding ulcer who, after surgical intervention and subsequent lifestyle adjustments, achieved long-term remission.
By understanding the comprehensive treatment options available, individuals can adopt a proactive approach to peptic ulcer management, thereby enhancing their health and quality of life.
Risk Factors for Peptic Ulcers
Peptic ulcers, which present as open sores on the inner lining of the stomach or upper part of the small intestine, manifest primarily due to the interplay of various risk factors. These risk factors encompass genetic predispositions, lifestyle choices, and certain medical conditions.
Genetic predisposition is a noteworthy element in the development of peptic ulcers. Individuals with a family history of peptic ulcers are at an elevated risk, suggesting a hereditary component. This genetic link underscores the importance of vigilance among those whose relatives have experienced these painful lesions.
Lifestyle choices significantly amplify the risk of peptic ulcers. Smoking, for instance, is a major contributor. Nicotine in cigarettes increases stomach acid production, which can harm the stomach lining. This is exemplified by numerous cases where heavy smokers have reported recurrent ulcer symptoms. Similarly, excessive alcohol consumption disrupts the mucosal barrier, leaving the stomach lining vulnerable to digestive acids. Chronic drinkers are therefore particularly susceptible to peptic ulcers.
Beyond lifestyle choices, certain medical conditions also predispose individuals to peptic ulcers. The presence of Helicobacter pylori bacteria is a well-documented risk factor. This bacterium disrupts the stomach’s protective lining and leads to inflammation, making it easier for ulcers to develop. Additionally, prolonged use of nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and aspirin, can irritate and inflame the stomach lining, increasing the risk of ulcers. Patients with conditions like rheumatoid arthritis, who often rely on NSAIDs, should be particularly cautious.
Real-life examples provide a clearer picture of how these risk factors interplay. For instance, a middle-aged individual with a family history of ulcers, who smokes and consumes alcohol regularly, would be at an extraordinarily high risk. Awareness of these contributing factors is essential for prevention. Adopting a healthier lifestyle, moderating alcohol intake, quitting smoking, and managing any underlying medical conditions can significantly reduce the risk, thus fostering better digestive health.
Lifestyle Modifications for Prevention and Management
Managing and preventing peptic ulcers often requires a comprehensive approach that incorporates lifestyle modifications. These changes can play a crucial role in both alleviating symptoms and preventing the recurrence of ulcers. Diet, stress management, and the elimination of risk factors such as smoking and excessive alcohol consumption are fundamental to this approach.
Dietary changes are among the most significant modifications one can make. Consuming a balanced diet rich in fruits, vegetables, and whole grains can bolster the gastrointestinal tract’s health. It is advisable to avoid spicy foods, caffeine, and foods high in fat, as these can exacerbate ulcer symptoms. Small, frequent meals can also help manage stomach acid levels, providing relief from discomfort.
Stress management is another vital component. Chronic stress may exacerbate peptic ulcer symptoms and impede the healing process. Techniques such as mindfulness, meditation, yoga, and deep-breathing exercises can significantly reduce stress levels. Incorporating regular physical activity, which also enhances overall well-being, can contribute to effective stress management.
Eliminating risk factors such as smoking and excessive alcohol consumption is essential. Smoking has been shown to increase stomach acid production, delay healing, and raise the risk of ulcer complications. Similarly, alcohol irritates the stomach lining and can worsen ulcer symptoms. By reducing or eliminating these habits, individuals can significantly improve their gastrointestinal health.
Real-life scenarios illustrate that these changes are feasible and beneficial. For example, one might start by gradually replacing morning coffee with herbal tea, integrating a 10-minute meditation session into their lunch break, or opting for a brisk walk after dinner instead of evening drinks. These small yet impactful decisions contribute to a healthier lifestyle and promote the healing of peptic ulcers.
By making these lifestyle modifications, individuals can take proactive steps in managing and preventing peptic ulcers, ultimately leading to better health and improved quality of life.