Introduction to Diverticulitis
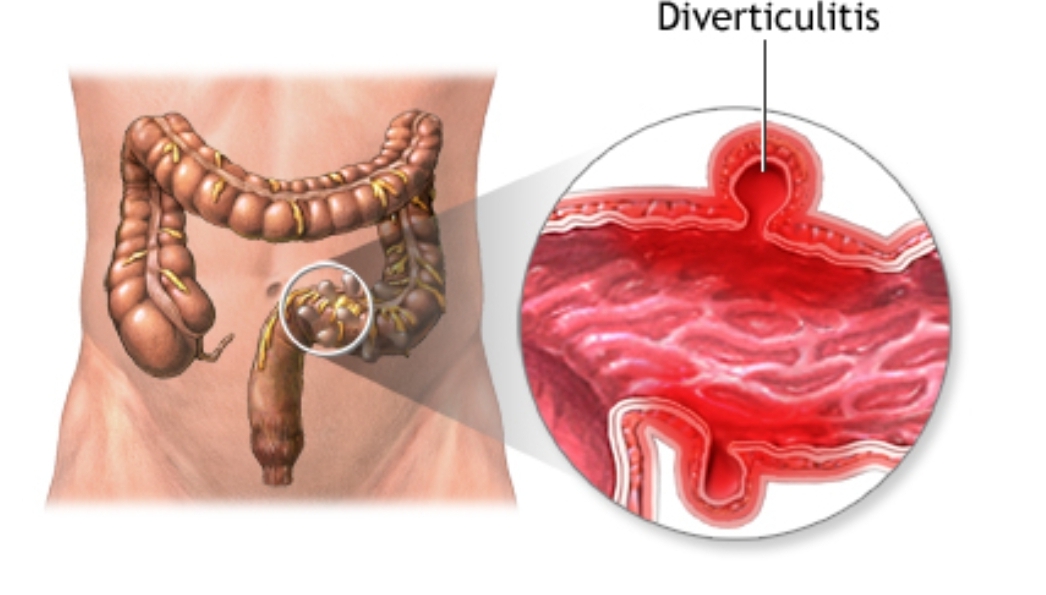
Diverticulitis is a relatively common gastrointestinal condition that affects many individuals, particularly as they age. To understand this condition, think of the colon, or large intestine, as a garden hose. Over time, small pouches or bulges, similar to dandelions sprouting on the hose’s exterior, may form along the colon. These small pouches are known as diverticula. When these diverticula become inflamed or infected, the condition is termed diverticulitis.
Diverticulitis can be an extremely painful and disruptive health issue. It ranks high in terms of gastrointestinal illnesses, particularly in Western societies where diets tend to be lower in fiber. Approximately 10% of Americans over the age of 40 are affected by diverticulitis, and this prevalence increases with age, rising to about 50% for those over the age of 60. This clearly indicates the importance of understanding diverticulitis, as it affects a substantial portion of the population.
Certain factors elevate the risk of developing diverticulitis. Age is the primary risk factor—older adults are significantly more likely to develop diverticula. A diet low in fiber, obesity, smoking, and a sedentary lifestyle are also contributing factors that increase susceptibility to this condition. Additionally, genetics play a role, meaning if a close family member has experienced diverticulitis, the likelihood of developing it is higher.
Grasping the fundamentals of diverticulitis is crucial for everyone, as early recognition and management can significantly improve health outcomes. Given its prevalence, awareness and knowledge about diverticulitis can help mitigate the potential severity of the condition. Throughout this comprehensive guide, we will delve deeper into its symptoms, causes, diagnostic methods, and treatment options to provide you with an extensive understanding of diverticulitis.
Causes of Diverticulitis
Diverticulitis is a complex condition influenced by a variety of factors. Understanding what causes diverticulitis can offer valuable insights into preventive measures. Primarily, lifestyle choices play a central role in the development of this condition. A diet low in fiber, for instance, is a significant contributor. Fiber aids in bowel movement regularity, and a deficiency can result in harder stools that are more difficult to pass, putting extra pressure on the colon walls. Over time, this added strain may lead to the formation of diverticula, small bulging pouches in the digestive tract that can become inflamed or infected, resulting in diverticulitis.
Consider a hypothetical scenario involving ‘John,’ an individual with a typically low-fiber diet. John’s daily meals rarely include fruits, vegetables, or whole grains, leaning heavily instead on processed foods. This dietary pattern not only slows his digestive process but also adds strain on his intestines, gradually leading to the development of diverticula.
Sedentary behavior further exacerbates this issue. John’s job requires him to sit for extended periods, reducing his overall physical activity. Regular exercise is vital for maintaining healthy bowel movements, and a lack of it can contribute to gastrointestinal problems. Prolonged inactivity coupled with poor dietary habits creates a perfect storm for diverticulitis onset.
Genetic predisposition is another crucial factor. While lifestyle choices are pivotal, some individuals may inherit a susceptibility to diverticulitis. If diverticulitis or other bowel conditions run in John’s family, he might be more prone to developing the condition regardless of his lifestyle. Thus, hereditary factors cannot be overlooked.
In summary, diverticulitis arises from a combination of a low-fiber diet, sedentary lifestyle, and genetic tendencies. By addressing these contributing factors—incorporating more fiber, increasing physical activity, and being aware of familial health history—individuals like John can better manage their risks associated with diverticulitis.
Signs and Symptoms of Diverticulitis
Diverticulitis is a condition marked by the inflammation or infection of small pouches, known as diverticula, that can form along the digestive tract. Understanding the signs and symptoms of diverticulitis is crucial for early diagnosis and effective management. Common symptoms include abdominal pain, fever, nausea, and changes in bowel habits. However, these symptoms can manifest differently across individuals, making it essential to be vigilant and seek medical advice if they occur.
Abdominal pain is often the most noticeable symptom. For some, like ‘Mary,’ the pain might start gradually in the lower left side of the abdomen, increasing in intensity over several days. She might initially dismiss it as minor discomfort, but over time, the pain can become severe and constant, making daily activities challenging. In other scenarios, such as ‘Tom’s case, the pain can be sudden and acute, necessitating immediate medical attention. This sudden onset can be unsettling and often indicates a more severe case of diverticulitis requiring prompt intervention.
Fever is another common symptom, typically indicating an infection. Accompanying this is often nausea and an overall feeling of malaise. These symptoms can sometimes be mistaken for less serious conditions such as the flu or food poisoning. However, when experienced alongside persistent abdominal pain, they warrant a closer investigation.
Changes in bowel habits, including both constipation and diarrhea, are frequently observed in those with diverticulitis. The inflammation caused by the condition can disrupt normal bowel movements, leading to discomfort and irregularity. It’s not unusual for individuals like Mary or Tom to notice their usual patterns are off, with bowel movements becoming painful or irregularly timed.
It is essential to recognize these symptoms early and seek medical attention. Ignoring them can lead to complications such as abscesses, perforation of the colon, or severe infection. If you or someone you know is experiencing these symptoms, a healthcare provider can offer proper diagnosis and treatment, ensuring better outcomes and preventing further complications.
Complications of Diverticulitis
Untreated diverticulitis can lead to significant complications, threatening both comfort and health. One of the most common complications is the formation of an abscess. An abscess is a pocket of infection that occurs when pus accumulates in the body’s tissues due to an infection. This condition can present with severe abdominal pain, fever, and swelling. In advanced cases, abscesses may require surgical drainage, highlighting the necessity of timely medical intervention.
Perforation of the colon is another severe complication of diverticulitis. Inflammatory processes can create a hole in the colon wall, allowing intestinal contents to spill into the abdominal cavity. This situation can result in peritonitis, a life-threatening inflammation of the abdominal lining. Symptoms include extreme abdominal pain, fever, and a rapid heartbeat. Immediate medical treatment is crucial to prevent widespread infection and other fatal outcomes.
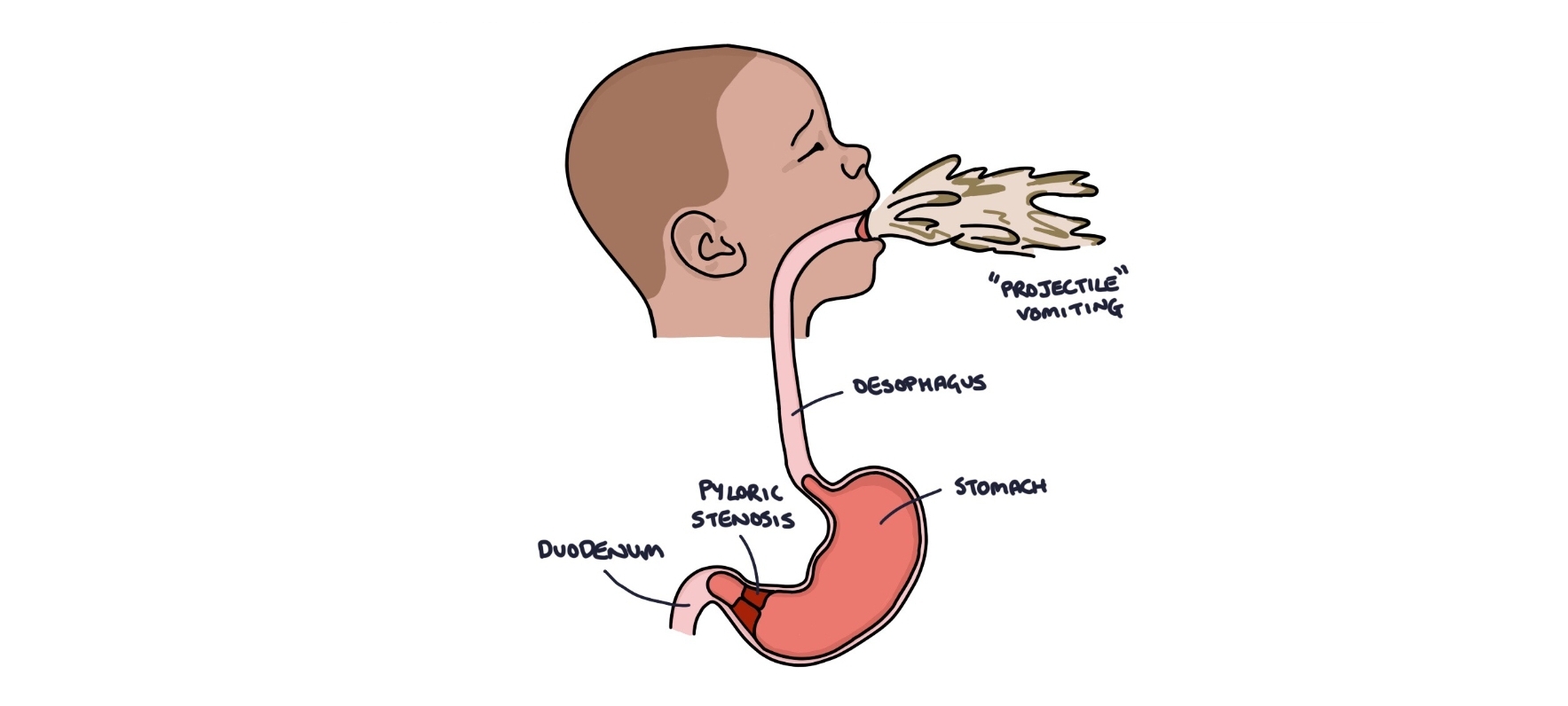
Moreover, diverticulitis can lead to intestinal obstruction. Chronic inflammation may cause parts of the intestine to narrow, obstructing the passage of food and waste. Patients with intestinal obstruction may experience nausea, vomiting, severe cramping, and an inability to pass gas or stool. Surgery is often required to alleviate the obstruction and restore normal bowel function.
Statistics underline the grave nature of these complications. According to a study published in the “Journal of Gastrointestinal Surgery,” approximately 25% of patients with acute diverticulitis develop complications such as abscesses, perforations, or obstructions. Furthermore, data from the American Society of Colon and Rectal Surgeons indicate that untreated diverticulitis has a mortality rate of over 5% due to severe complications like peritonitis.
Ignoring the symptoms of diverticulitis can ultimately result in catastrophic health events. Real-life case studies emphasize the urgency—patients suffering from untreated diverticulitis have experienced prolonged hospital stays, multiple surgeries, and extensive recovery periods. Thus, fostering awareness and encouraging prompt medical attention is crucial in mitigating the risks associated with this condition.
Pathophysiology of Diverticulitis
Diverticulitis originates from diverticula, which are small bulging pouches that can form in the lining of the digestive system. Primarily, they are found in the lower part of the large intestine, also known as the colon. The formation of these pouches, termed diverticulosis, can be attributed to certain physiological and biological changes within the colon.
The development of diverticula usually begins with the weakening of the colon’s wall. Several factors like diet low in fiber, aging, and increased intraluminal pressure contribute to this wall weakening. Imagine your colon as a long balloon; when internal pressure increases beyond a certain point, the weakened spots begin to bulge out, creating diverticula. These pocket-like structures, though often harmless on their own, can turn problematic under certain conditions.
Diverticulitis occurs when these pouches become inflamed or infected. This inflammation is often caused by a blockage at the opening of the diverticula. Just like a small wound on your skin that can become infected if dirt gets into it, the diverticula can become inflamed if small particles of stool or bacteria are trapped inside. This blockage can lead to increased pressure, decreased blood flow, and ultimately, inflammation. Bacteria trapped within the pouches can proliferate, causing an infection to develop.
The body’s immune response to this infection sets off a series of events resulting in inflammation. White blood cells and other immune components rush to the site to combat the infection, leading to swelling, redness, and pain in the affected area. The inflammatory process can sometimes create a cycle, causing further complications such as abscesses or perforations in severe cases.
In summary, understanding diverticulitis involves acknowledging how these small pouches form in the colon, how they can become inflamed, and recognizing the body’s response to such infections. Through this detailed insight, one can better appreciate the intricate processes that underlie this common yet complex condition.
Diagnosis of Diverticulitis
The diagnostic process for diverticulitis begins with a thorough medical history and physical examination. During the medical history intake, a physician inquires about the patient’s symptoms, dietary habits, and any pertinent past medical issues. This step is essential to identify common risk factors associated with diverticulitis, such as age and family history.
Following the history gathering, a physical examination takes place, where the physician palpates the abdomen to check for tenderness, particularly in the lower left quadrant, which is a typical site of discomfort in diverticulitis cases. Additional signs such as fever, bloating, and changes in bowel habits might also be evaluated.
To confirm the diagnosis, various diagnostic tests are employed. A computed tomography (CT) scan is often the definitive test. It provides a detailed image of the colon and can reveal inflamed or infected diverticula, as well as complications like abscesses or perforations. Patients undergoing a CT scan may experience the quick, non-invasive process that involves lying on a table while the scanner takes cross-sectional images of the body.
In some cases, a colonoscopy may be recommended post-infection to assess the extent of diverticular disease and rule out other conditions, such as colorectal cancer. This procedure involves the insertion of a flexible tube with a camera into the colon, and patients need to prepare by following a clear liquid diet and taking a bowel-cleansing solution the day before.
Additionally, blood tests play a critical role in the diagnostic process. Elevated white blood cell counts can indicate infection or inflammation, supporting the suspicion of diverticulitis. However, these blood tests alone cannot confirm the diagnosis but contribute to a comprehensive evaluation.
Distinguishing diverticulitis from other gastrointestinal disorders, such as irritable bowel syndrome (IBS) or acute appendicitis, is crucial. For instance, the location of abdominal pain and associated symptoms like changes in stool consistency can help differentiate conditions. Overall, a combination of medical history, physical examinations, and targeted diagnostic tests enables healthcare providers to accurately diagnose and manage diverticulitis, ensuring effective treatment and care for patients.
Management and Treatment
Diverticulitis, an inflammation of the digestive tract’s pouches, requires a multifaceted approach for effective management and treatment. Options for addressing this condition range widely, depending on the severity of the symptoms and the individual’s overall health. Early intervention often focuses on conservative treatments, which can significantly deter the progression of diverticulitis.
Initially, lifestyle changes and dietary modifications are essential. Increasing fiber intake is a cornerstone of diverticulitis prevention and management. For instance, Jane, a patient diagnosed with diverticulitis, experienced considerable symptom relief by incorporating more fruits, vegetables, and whole grains into her diet. These high-fiber foods help to soften and add bulk to the stool, reducing the pressure on the colon walls and preventing further complications.
In contrast to dietary adjustments, medical management may be necessary, particularly for acute episodes of diverticulitis. Antibiotics are commonly prescribed to combat inflammation and infection. Mild cases frequently respond well to these medications, enabling many individuals to avoid more invasive procedures. Over-the-counter pain relievers can provide symptom relief, but it is important to consult with a healthcare provider to ensure they do not exacerbate the condition.
For those with severe or recurrent episodes, surgical intervention might be required. Richard’s story illustrates a successful outcome from surgery. After several acute attacks, he underwent a procedure to remove the affected portion of his colon. Post-surgery, Richard adhered to a prescribed health regimen, including follow-up care, which was pivotal for his recovery. This underscores the necessity of monitoring and ongoing support for patients recovering from diverticulitis. Regular check-ups and adherence to a tailored medical plan can vastly improve long-term outcomes.
Conclusively, while treating diverticulitis can be complex, a combination of dietary changes, medication, and possibly surgery, complemented by diligent follow-up care, enhances recovery and minimizes recurrence. Each approach needs to be individualized, ensuring patients receive the most effective care tailored to their specific needs.
Living with Diverticulitis
Living with diverticulitis requires a multifaceted approach that includes dietary adjustments, regular exercise, and effective stress management. Managing this condition long-term is essential for reducing flare-ups and improving quality of life. Below, we delve into practical tips and advice for living with diverticulitis successfully.
One of the fundamental aspects of managing diverticulitis is adopting a suitable diet. Typically, a high-fiber diet is recommended to keep the digestive system functioning smoothly. Foods rich in fiber such as vegetables, fruits, whole grains, and legumes help soften stool and facilitate its passage through the bowel, thereby reducing pressure on the diverticula. It’s also vital to stay hydrated by drinking plenty of water throughout the day to aid digestion.
Regular exercise plays a crucial role in maintaining digestive health. Activities like walking, swimming, and yoga can enhance bowel function and prevent constipation, a common issue that aggravates diverticulitis. Incorporating at least 30 minutes of moderate exercise most days of the week can make a significant difference. For example, John, a diverticulitis patient, found that walking his dog every morning not only helped with his symptoms but also improved his overall wellbeing.
Stress can have a profound impact on diverticulitis. Stress management techniques such as mindfulness, meditation, and deep-breathing exercises can help mitigate stress-related flare-ups. Jane, another patient, mentioned that practicing yoga and meditation significantly reduced her episodes of diverticulitis, making these activities an integral part of her daily routine.
The role of support groups and access to resources cannot be understated. Connecting with others who have diverticulitis provides emotional support and practical advice. Online forums, local support groups, and consultations with healthcare professionals can offer valuable insights and coping strategies. The Sharing Strength support group, for instance, offers a platform where individuals share their journeys and success stories, fostering a sense of community and shared understanding.
In conclusion, managing diverticulitis effectively involves a combination of proper diet, regular physical activity, stress management, and support from others. By integrating these strategies, individuals can lead fulfilling lives while minimizing the impact of diverticulitis.