Introduction to Pyloric Stenosis
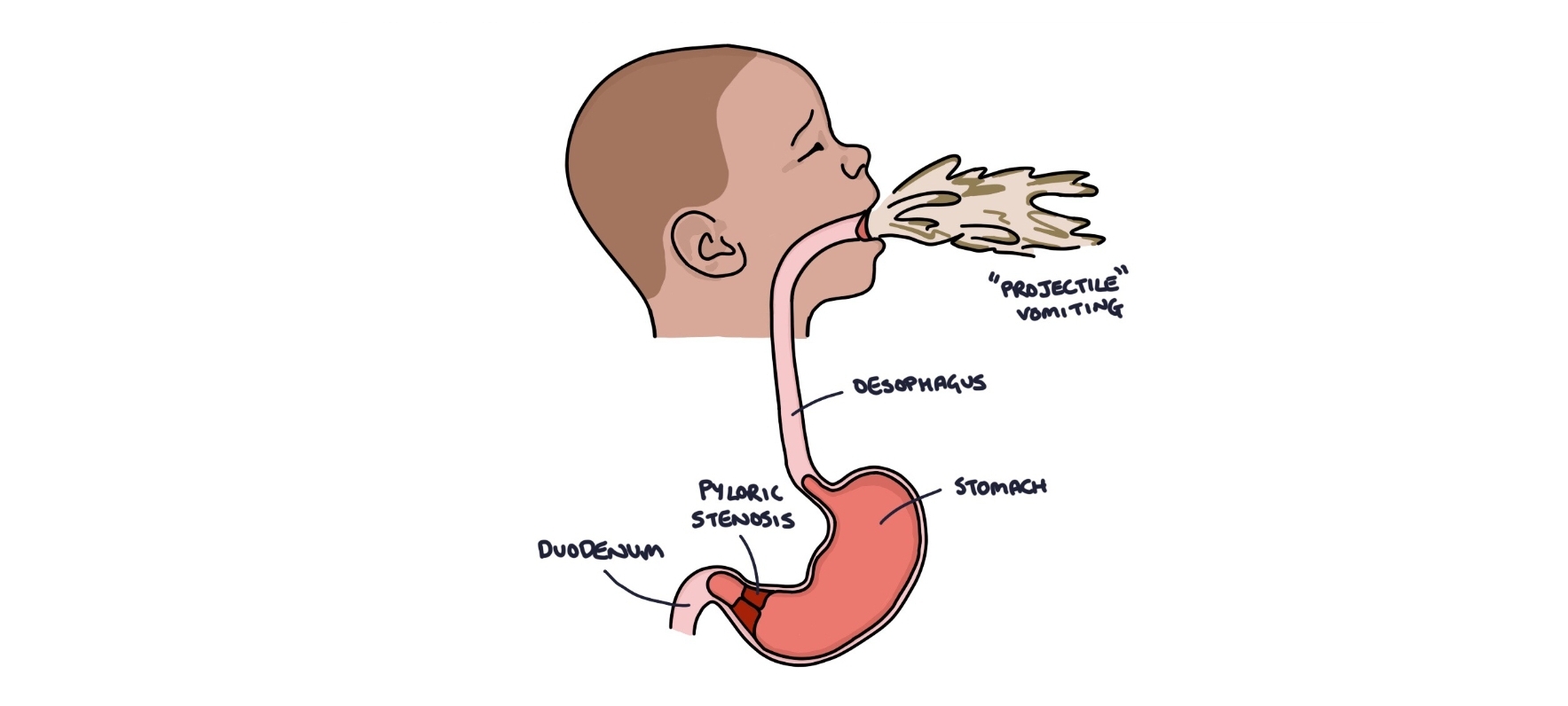
Pyloric stenosis is a condition characterized by the narrowing of the pylorus, which is the opening between the stomach and the small intestine. This narrowing can lead to significant obstruction, ultimately hindering the passage of food from the stomach into the small intestine. Predominantly affecting infants, pyloric stenosis manifests usually between three to twelve weeks of age. The precise causes of this condition are not fully understood, though genetic factors and environmental influences may play a role.
In a healthy digestive system, food moves smoothly from the stomach to the intestine, where it is further digested and absorbed. In cases of pyloric stenosis, the hypertrophy of the pyloric muscle creates a barrier, leading to vomiting, dehydration, and electrolyte imbalances. Parents often notice projectile vomiting in their infant, which can be alarming and prompts medical evaluation. Understanding the intricacies of this condition is critical, especially for caregivers and healthcare professionals.
Through the use of real-life scenarios, it becomes easier to grasp the implications of pyloric stenosis in day-to-day life. Describing experiences that parents face, such as the emotional strain of seeing their child struggle with feeding, can help demystify medical jargon. This narrative approach not only engages the audience but also highlights the significance of timely diagnosis and treatment, which can greatly improve the prognosis for affected infants. By making complex medical concepts accessible, these scenarios can foster empathy and understanding among readers.
As we explore the causes, pathophysiology, complications, and symptoms associated with pyloric stenosis, a comprehensive understanding of this condition will emerge. This knowledge is essential for identifying symptoms early and facilitating effective treatments.
Real-life Scenario: The First Signs of Pyloric Stenosis
Jane and Michael, parents of a three-month-old infant named Lucas, began to notice something concerning about their son’s health. Although Lucas had initially been a happy and healthy baby, a sudden change in his behavior prompted them to seek medical advice. The first alarming sign was projectile vomiting. Instead of spitting up following feedings, Lucas would expel his formula forcefully, sending it several feet across the room. This unusual and dramatic vomiting was accompanied by a ravenous appetite; immediately after vomiting, Lucas would cry vigorously, indicating he was still hungry.
Along with the vomiting, Jane observed that Lucas was becoming increasingly dehydrated. His normally moist diaper changed to a much dryer state, and he developed noticeable lethargy. Jane was well aware of the signs of dehydration, which can be particularly dangerous for infants. It was particularly distressing for the couple to see their baby’s energy levels decline, as he seemed less active and less engaged. They monitored Lucas closely, and each time he vomited, their concern deepened.
The couple’s anxieties heightened when they noticed Lucas struggling to keep any food down. After a particularly distressing night of frequent vomiting, Jane and Michael decided to take him to the pediatrician for a thorough examination. The physician recognized the classic symptoms associated with pyloric stenosis during the examination, including physical signs like an empty stomach area and the olive-shaped mass that is often felt in the abdomen. This experience illustrated the emotional rollercoaster faced by parents when they witness such concerning signs, ultimately leading them to seek immediate medical care for their child.
Causes of Pyloric Stenosis
Pyloric stenosis is a condition characterized by the narrowing of the pylorus, which is the opening between the stomach and the small intestine. While the exact causes remain largely unknown, several factors have been identified that may contribute to the development of this gastrointestinal disorder. Research suggests a strong genetic predisposition, with pyloric stenosis appearing more frequently among family members of affected individuals. A notable demographic trend indicates that this condition predominantly affects infants, especially those who are firstborn. As illustrative examples, consider a scenario where a firstborn child presents with symptoms such as vomiting and excessive hunger; these may be direct ramifications of pyloric stenosis, indicating the condition’s significance in this demographic.
Environmental factors may also play a role in the manifestation of pyloric stenosis. Some studies highlight the potential influence of maternal smoking during pregnancy, suggesting that exposure to tobacco could increase the risk of developing the condition. Additionally, factors such as gestational age and certain maternal health conditions have been examined for their connections to pyloric stenosis, although conclusive links remain to be fully established.
Furthermore, male infants are at a higher risk compared to females, with some research indicating that the male-to-female ratio can be as high as 4:1. Understanding these demographic and environmental trends is crucial for healthcare professionals who suspect pyloric stenosis in their patients, particularly in the case of firstborn males. By recognizing these patterns, early diagnosis and intervention can be facilitated, ultimately leading to improved outcomes for affected infants.
The Pathophysiology of Pyloric Stenosis
Pyloric stenosis is a condition characterized by the abnormal narrowing of the pylorus, the outlet of the stomach that leads into the small intestine. The pathophysiology of this condition primarily involves hypertrophy, or the excessive growth, of the smooth muscle surrounding the pylorus. This growth results in a significant reduction in the diameter of the pyloric channel, which ultimately impedes the passage of gastric contents into the duodenum.
The etiology of pyloric stenosis remains somewhat unclear, but it is believed that genetic and environmental factors contribute to its development. In infants, the muscle tissue in the pylorus may respond abnormally during critical periods of growth, leading to the thickening of these smooth muscle fibers. As the muscle hypertrophies, it creates a blockage that prevents food and digestive juices from properly moving from the stomach to the intestine, which is crucial for normal digestion.
This obstruction leads to delayed gastric emptying, resulting in symptoms such as projectile vomiting, dehydration, and poor weight gain. Over time, the accumulation of gastric contents can increase intra-gastric pressure, further exacerbating the retention and leading to abdominal distension. These physiological disturbances can also have cascading effects on electrolytes and metabolic functions, creating potential complications such as metabolic alkalosis and electrolyte imbalances.
Understanding the pathophysiological processes behind pyloric stenosis is vital for medical professionals in diagnosing and managing the condition. Due to the narrowed pylorus, therapeutic interventions often involve surgical procedures, such as a pyloromyotomy, to relieve the obstruction and restore normal gastric function. Recognizing the signs early in infants is crucial, as timely intervention can significantly improve outcomes and facilitate healthy growth and development.
Real-life Scenario: Impact on Infant Development
Consider the case of a six-week-old infant named Lucas, who appeared healthy at birth but soon began to exhibit signs of distress. Lucas’s parents noted his persistent vomiting after feeding, leading to concerns about his ability to gain weight. Each instance of vomiting left the infant appearing hungry yet unable to retain nutrients, causing significant anxiety for his parents. This scenario is a classic representation of how pyloric stenosis can drastically affect an infant’s growth and development.
The underlying cause of Lucas’s symptoms was identified as pyloric stenosis, a condition that obstructs the passage between the stomach and small intestine. Despite being born without complications, the gradual onset of projectile vomiting denied him essential calories for growth, impacting his physical health. This compounded his inability to thrive, leading to frustration and helplessness among his caregivers. Regular pediatric consultations highlighted the importance of early diagnosis and intervention, as prolonged malnutrition could stifle his development in critical milestones.
The psychosocial dynamics of managing pyloric stenosis cannot be underestimated. Lucas’s parents often felt overwhelmed, grappling with their child’s discomfort while simultaneously worrying about his growth trajectory. The emotional toll was palpable, resulting in stress-induced strain in their relationship. Parents experiencing similar situations often report feelings of isolation, as the very core of their nurturing instincts is challenged by their baby’s condition. The struggles they faced underscore the multifaceted issues surrounding pyloric stenosis—encompassing both its physical repercussions on infant development and the emotional burdens that accompany parental care and concern.
Through Lucas’s story, we see how pyloric stenosis manifests not just as a medical condition but also as a significant factor influencing family dynamics and infant growth. Addressing both physical ailments and emotional aspects is crucial in the comprehensive management of this infantile disorder.
Complications of Pyloric Stenosis
Pyloric stenosis, if left untreated, can lead to a variety of serious complications that may significantly impact a patient’s health. One of the most critical complications is severe dehydration. As the pylorus—the opening from the stomach to the small intestine—narrows, it restricts food and liquids from passing through effectively. This obstruction often leads to excessive vomiting, which can rapidly deplete the body’s fluids. For infants, who are particularly vulnerable, severe dehydration can escalate quickly, causing extreme fatigue, irritability, and lethargy. Parents should be observant of any signs of dehydration, such as dry mouth, decreased urine output, or unusual fussiness.
Another notable complication resulting from untreated pyloric stenosis is electrolyte imbalances. The vomiting associated with the condition can lead to significant losses of essential electrolytes such as sodium, potassium, and chloride. These imbalances can disturb various bodily functions and, if severe, may necessitate urgent medical intervention. For example, low potassium levels can cause muscle weakness and heart rhythm disturbances, which can be life-threatening. In our previous scenarios, it was evident how quickly the symptoms escalated; one child went from mild vomiting to exhibiting signs of dehydration and weakness in just a few days.
Aside from dehydration and electrolyte imbalances, untreated pyloric stenosis can lead to malnutrition, as infants are unable to absorb adequate nutrients. Persistent obstruction may cause a failure to thrive, with noticeable weight loss and growth delays. Hence, parents and caregivers should be vigilant about their child’s feeding patterns and any abnormal symptoms, including frequent vomiting or changes in behavior. Prompt medical attention is vital when pyloric stenosis is suspected, as early intervention can significantly reduce the risk of these complications. The swift action taken in such scenarios can provide the necessary care to restore the health and well-being of the affected child.
Trademark Signs and Symptoms
Pyloric stenosis is a gastrointestinal condition that primarily affects infants, characterized by the narrowing of the pylorus, which is the opening from the stomach into the small intestine. One of the most pronounced symptoms of this condition is projectile vomiting, which typically occurs shortly after feeding. This form of vomiting is notably forceful and can result in the infant expelling a considerable amount of gastric contents over a considerable distance. It is crucial for caregivers to monitor such occurrences, as they can indicate the presence of pyloric stenosis, necessitating immediate medical intervention.
Another significant symptom is constant hunger. Many infants with pyloric stenosis may appear to feed frequently, showing signs of hunger shortly after vomiting. This can create a cycle where the infant consumes more food, only to vomit it back up, creating a concerning scenario for caregivers. Recognizing this pattern of excessive feeding coupled with vomiting assists in early identification of potential pyloric stenosis and emphasizes the need for parental vigilance.
Additionally, a distinctive physical sign associated with pyloric stenosis is the presence of an ‘olive’ mass in the abdomen. Upon examination, a healthcare professional may palpate a firm, mobile, and oval-shaped mass in the right upper quadrant of the abdomen. This mass is essentially the hypertrophied pylorus and represents an important clinical finding in the diagnosis of this condition. Parents should be informed that if their infant presents with projectile vomiting, constant hunger, and abdominal distension along with this olive-shaped mass, seeking prompt medical evaluation is imperative.
Understanding these hallmark symptoms can greatly enhance the likelihood of early diagnosis and treatment, thereby reducing the risk of complications associated with pyloric stenosis. Observing these signs closely ensures that caregivers are prepared to act swiftly in response to possible indicators of this serious condition.
Diagnostic Approaches for Pyloric Stenosis
Detecting pyloric stenosis requires a combination of thorough clinical evaluation and imaging techniques. The first step in the diagnostic process typically involves a comprehensive physical examination conducted by a healthcare provider. During this examination, the physician will assess the infant for key signs of pyloric stenosis, such as projectile vomiting, dehydration, and significant weight loss. In many cases, a palpable “olive” mass in the right upper quadrant of the abdomen may be felt, indicating hypertrophy of the pylorus.
Following the physical examination, ultrasound imaging is the gold standard for confirming the diagnosis. Abdominal ultrasound is a non-invasive, safe, and effective tool that allows physicians to visualize the pyloric channel’s thickness and length. A thickened pylorus, generally measuring greater than 4 mm in muscle wall thickness, is a hallmark of pyloric stenosis. The ultrasound can also reveal abnormal peristalsis and gastric outlet obstruction, which are critical in substantiating the diagnosis.
In addition to ultrasound, laboratory tests may be employed to assess the infant’s hydration status and electrolyte balance. These tests often include complete blood count (CBC) and metabolic panel analyses to evaluate for metabolic alkalosis or dehydration, common in infants with pyloric stenosis due to persistent vomiting. Early detection is paramount, as prompt diagnosis facilitates timely intervention, which can significantly improve outcomes for the infant.
As discussed in the scenarios referenced earlier, recognizing the signs of pyloric stenosis soon after they arise allows healthcare providers to make informed decisions regarding treatment options. Timely intervention is crucial in preventing complications such as electrolyte imbalances or surgical emergencies. Ultimately, the integration of thorough physical assessments, advanced imaging techniques, and laboratory evaluations forms the cornerstone of accurate and timely diagnostic approaches for pyloric stenosis.
Treatment Options and Prognosis
Treatment for pyloric stenosis primarily revolves around surgical intervention, specifically a procedure known as pyloromyotomy. This surgery aims to relieve the obstruction caused by the thickened pylorus, allowing food to pass freely from the stomach to the small intestine. It is typically performed under general anesthesia and involves incising the muscle of the pylorus to widen its opening without removing any tissue. The procedure is generally straightforward and has an excellent success rate, with most infants experiencing significant improvement shortly after surgery.
Prior to surgical intervention, most infants require stabilization, which often includes intravenous fluids and electrolyte replenishment to address dehydration and imbalanced electrolytes resulting from persistent vomiting. This preparatory phase is crucial to ensure that the infant is in optimal condition for surgery, thereby reducing the risk of complications during the procedure.
While the surgical approach is the primary treatment, parents and caregivers of affected infants can take comfort in the positive prognosis post-treatment. Following pyloromyotomy, the majority of infants show remarkable recovery, returning to normal feeding patterns within a few days. For instance, in one real-life scenario, after undergoing surgery, a young patient demonstrated significant progress within 48 hours, transitioning from intravenous nourishment to oral feeds effectively. This transformation not only alleviated the immediate concerns of the family but also marked the beginning of a healthy growth trajectory.
Complications from the surgery are rare but can include infections or bleeding. Nevertheless, the overall outcomes are overwhelmingly favorable, with most children recovering fully and leading normal lives. Pyloric stenosis, when addressed promptly with surgery, tends to have an excellent long-term outlook, reinforcing the importance of early diagnosis and timely treatment for improving the life quality for affected families.