Introduction to Gaucher Disease
Gaucher Disease is a rare genetic disorder that can be difficult to understand without a medical background. To simplify, imagine your body as a well-organized library. In this library, every book (or cell) has a specific place and function. Now, think of Gaucher Disease as a scenario where certain books are misplaced, causing confusion and disorder. Specifically, it occurs when the body lacks an enzyme called glucocerebrosidase, which helps break down a fatty substance known as glucocerebroside. Without this enzyme, glucocerebroside accumulates in cells, leading to various symptoms and complications.
Gaucher Disease can be categorized into three main types: Type 1, Type 2, and Type 3. Type 1 is the most common and does not affect the nervous system, while Types 2 and 3 do. Symptoms can range from mild to severe and may include enlarged liver and spleen, anemia, bone pain, and fatigue. It’s important to note that these symptoms can vary greatly from person to person, making diagnosis and treatment a complex process.
To help remember the key points about Gaucher Disease, we can use a simple mnemonic: “G-A-U-C-H-E-R.” – **G** – Glucocerebrosidase deficiency- **A** – Accumulation of glucocerebroside- **U** – Uncommon (rare genetic disorder)- **C** – Categories (Type 1, Type 2, Type 3)- **H** – Hepatosplenomegaly (enlarged liver and spleen)- **E** – Enzyme replacement therapy (a common treatment)- **R** – Range of symptoms (from mild to severe)
This mnemonic can serve as a helpful tool for both medical professionals and laypersons to recall the essential aspects of Gaucher Disease. Understanding these basics is the first step in recognizing the importance of early diagnosis and appropriate treatment options for those affected by this condition.
How Gaucher Disease Affects the Body
Gaucher Disease is a rare genetic disorder that can have a profound impact on various parts of the body. To understand its effects, imagine your body as a finely tuned car engine. In a well-functioning engine, all parts work seamlessly together to ensure smooth operation. However, if the engine’s filter becomes clogged, it disrupts the entire system, leading to inefficiencies and potential breakdowns. Similarly, Gaucher Disease disrupts normal bodily functions due to the accumulation of certain fatty substances called glucocerebrosides.
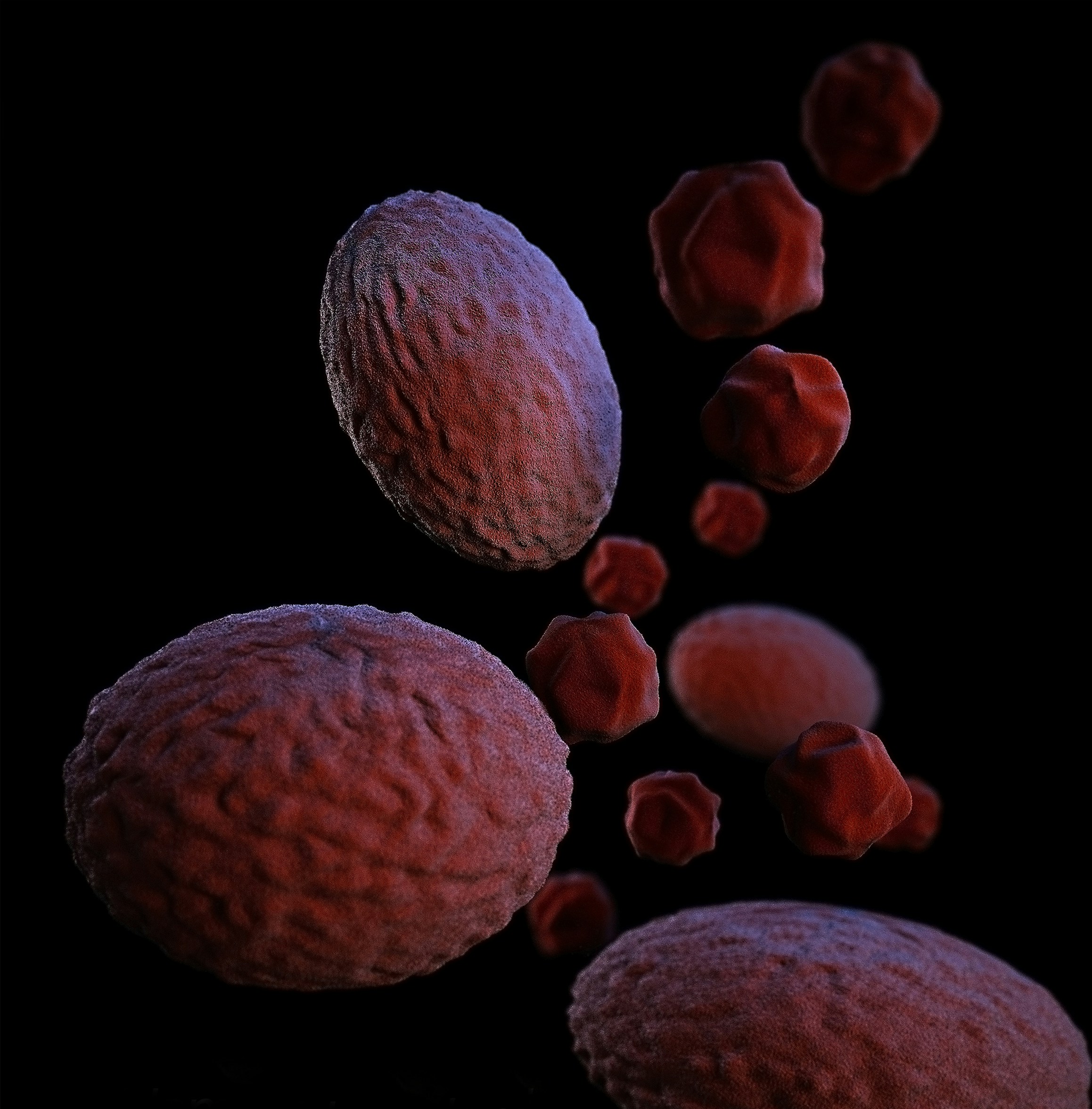
The build-up of these substances primarily affects the spleen, liver, and bone marrow. In the spleen, the accumulation can cause it to enlarge significantly, a condition known as splenomegaly. This can lead to discomfort and a feeling of fullness in the abdomen. The liver may also become enlarged (hepatomegaly), which can result in abdominal pain and a range of digestive issues.
Bone marrow, where blood cells are produced, is another critical area impacted by Gaucher Disease. The accumulation of glucocerebrosides can interfere with the production of healthy blood cells, leading to anemia, fatigue, and an increased risk of bleeding and bruising. Bone pain and fractures are also common symptoms due to the weakened structure of the bones.
To make these symptoms easier to remember, here’s a short rhyme:
“When the body’s filter clogs, it isn’t just a fog, The spleen and liver swell, making life a living hell, Bones ache and blood runs thin, it’s a battle from within.”
By understanding these impacts, we can better grasp the challenges faced by those with Gaucher Disease and emphasize the importance of early diagnosis and treatment to manage symptoms and improve quality of life.
Causes and Risk Factors
Gaucher Disease is primarily caused by genetic mutations in the GBA gene, which is responsible for producing the enzyme glucocerebrosidase. This enzyme is crucial for breaking down a fatty substance called glucocerebroside within lysosomes, the waste disposal units in cells. When the GBA gene is mutated, the enzyme is either deficient or dysfunctional, leading to the accumulation of glucocerebroside in various tissues and organs, causing the symptoms associated with Gaucher Disease.
Inheritance of Gaucher Disease follows an autosomal recessive pattern. This means that an individual must inherit two defective copies of the GBA gene, one from each parent, to manifest the disease. If both parents are carriers—each possessing one mutated and one normal gene—there is a 25% chance with each pregnancy that their child will have Gaucher Disease, a 50% chance the child will be a carrier, and a 25% chance the child will inherit two normal genes.
Understanding family genetics can be simplified using a family tree or pedigree chart. For instance, if both parents are carriers (GBA+/GBA-), their children will have a range of genetic outcomes. By plotting these probabilities on a pedigree chart, it becomes easier to visualize how the disease can be passed on through generations.
Risk factors for Gaucher Disease are largely genetic. Individuals with Ashkenazi Jewish heritage have a higher prevalence of Gaucher Disease, with a carrier frequency of approximately 1 in 15. However, it is important to note that Gaucher Disease can affect individuals from any ethnic background.
To aid in remembering the key causes and risk factors, consider the mnemonic “GBA”—Gene mutation, Both parents must be carriers, and Ashkenazi Jewish heritage as a notable risk factor. This mnemonic encapsulates the crucial elements that lead to the development and inheritance of Gaucher Disease.
Diagnosing Gaucher Disease
Diagnosing Gaucher Disease can often feel like trying to find a needle in a haystack. The process typically begins with a visit to a healthcare provider who will conduct a thorough medical history and physical examination. This initial step is crucial, as Gaucher Disease symptoms can be diverse and mimic other conditions, making accurate diagnosis challenging.
The journey usually progresses to a series of blood tests. One of the primary tests is the enzyme assay, which measures the activity of the glucocerebrosidase enzyme. Low levels of this enzyme are indicative of Gaucher Disease. This test is often complemented by genetic testing, which looks for mutations in the GBA gene. Identifying these mutations can confirm the diagnosis and provide insight into the specific type of Gaucher Disease.
In some cases, imaging studies such as MRI or CT scans may be employed to assess the extent of organ involvement, particularly the liver and spleen. These scans provide a detailed view, allowing doctors to see the internal landscape and identify any abnormalities. Bone marrow biopsy might also be recommended if there’s suspicion of significant bone marrow involvement, although this is less common.
Practical scenarios help illustrate these diagnostic steps. Imagine visiting your doctor because of persistent fatigue, bone pain, or an enlarged abdomen. After discussing your symptoms, your doctor orders a blood test. The results show low enzyme activity, prompting further genetic testing. When the GBA gene mutation is identified, your doctor confirms you have Gaucher Disease and outlines the next steps for managing the condition.
Understanding the diagnostic process for Gaucher Disease is essential, as early and accurate diagnosis can significantly impact treatment and management. By breaking down these steps, we aim to make the complexities of Gaucher Disease more accessible and less daunting for patients and their families.
Treatment Options
Gaucher Disease, a genetic disorder, can be managed through several medical interventions, each designed to address the root cause of the condition. The primary treatment options include enzyme replacement therapy (ERT) and substrate reduction therapy (SRT). Let’s delve into these treatments in simple terms.
Enzyme replacement therapy (ERT) is akin to refilling a car’s oil. In Gaucher Disease, the body lacks a specific enzyme needed to break down certain fatty substances. ERT involves regular infusions of this missing enzyme, helping the body to process these substances properly. Think of it as giving your car the oil it needs to run smoothly. Commonly used ERT medications include imiglucerase, velaglucerase alfa, and taliglucerase alfa. These treatments have proven effective in alleviating many symptoms of Gaucher Disease, such as anemia, bone pain, and enlarged organs.
Substrate reduction therapy (SRT), on the other hand, aims to reduce the production of the fatty substances that accumulate in the cells of individuals with Gaucher Disease. It’s like cutting down on the oil consumption of a car to ensure it doesn’t run out too quickly. SRT medications, such as eliglustat and miglustat, work by inhibiting the production of glucocerebroside, the fatty substance that builds up due to the enzyme deficiency. This approach is particularly beneficial for those who may not respond well to ERT or prefer an oral medication.
Beyond these primary treatments, other interventions may include bone marrow transplantation, which can offer a potential cure but comes with significant risks, and supportive treatments to manage specific symptoms. For example, medications to manage bone pain, blood transfusions for anemia, and surgery for spleen removal may be considered based on individual needs.
In a nutshell, managing Gaucher Disease requires a tailored approach, balancing the benefits and risks of each treatment option:
Enzyme replacement, refilling the oil,Substrate reduction, keeping it loyal.
Each with its role, to ease the strain,Helping those with Gaucher, to live without pain.
Living with Gaucher Disease
Managing Gaucher Disease in daily life requires a combination of medical treatment, lifestyle adjustments, and a strong support system. Individuals living with Gaucher Disease can lead fulfilling lives by adopting certain strategies to cope with the symptoms and challenges of the condition.
One critical aspect of managing Gaucher Disease is adhering to a prescribed treatment regimen. Enzyme replacement therapy (ERT) and substrate reduction therapy (SRT) are common treatments that help manage the disease’s symptoms. Regular medical check-ups and consultations with a healthcare provider are essential to monitor the condition and adjust treatments as necessary.
Incorporating a healthy diet and regular exercise into daily routines can significantly impact quality of life. Maintaining a balanced diet rich in nutrients helps support overall health, while low-impact exercises, such as swimming or walking, can improve mobility and reduce fatigue. It is important to consult with a healthcare professional before starting any new diet or exercise program.
To help remember key lifestyle adjustments, consider the mnemonic “CARE”:
C: Consistent medical care
A: Active lifestyle with appropriate exercise
R: Regular, balanced diet
E: Emotional support from family, friends, and support groups
Emotional and mental health is just as important as physical health. Joining support groups or connecting with others who have Gaucher Disease can provide valuable emotional support and practical advice. These connections help individuals feel less isolated and more empowered to manage their condition.
Regular medical care is the cornerstone of managing Gaucher Disease. Just as a well-tended garden flourishes, so does the health of an individual who consistently follows their treatment plan and attends medical appointments. This proactive approach ensures that any changes in the condition are promptly addressed, allowing for timely interventions and adjustments to the treatment plan.
By integrating these strategies and maintaining a proactive approach to healthcare, individuals with Gaucher Disease can lead active, fulfilling lives. The journey may have its challenges, but with the right support and management, it is entirely possible to navigate life successfully with Gaucher Disease.