Introduction to Sandhoff Disease
Imagine a vibrant, energetic child who suddenly starts experiencing unexplained muscle weakness and loses the ability to crawl or sit up. Over time, this child may also begin to lose the ability to see and hear, and their mental development may start to regress. This heartbreaking scenario illustrates the impact of Sandhoff Disease, a rare genetic disorder that primarily affects the brain and spinal cord.
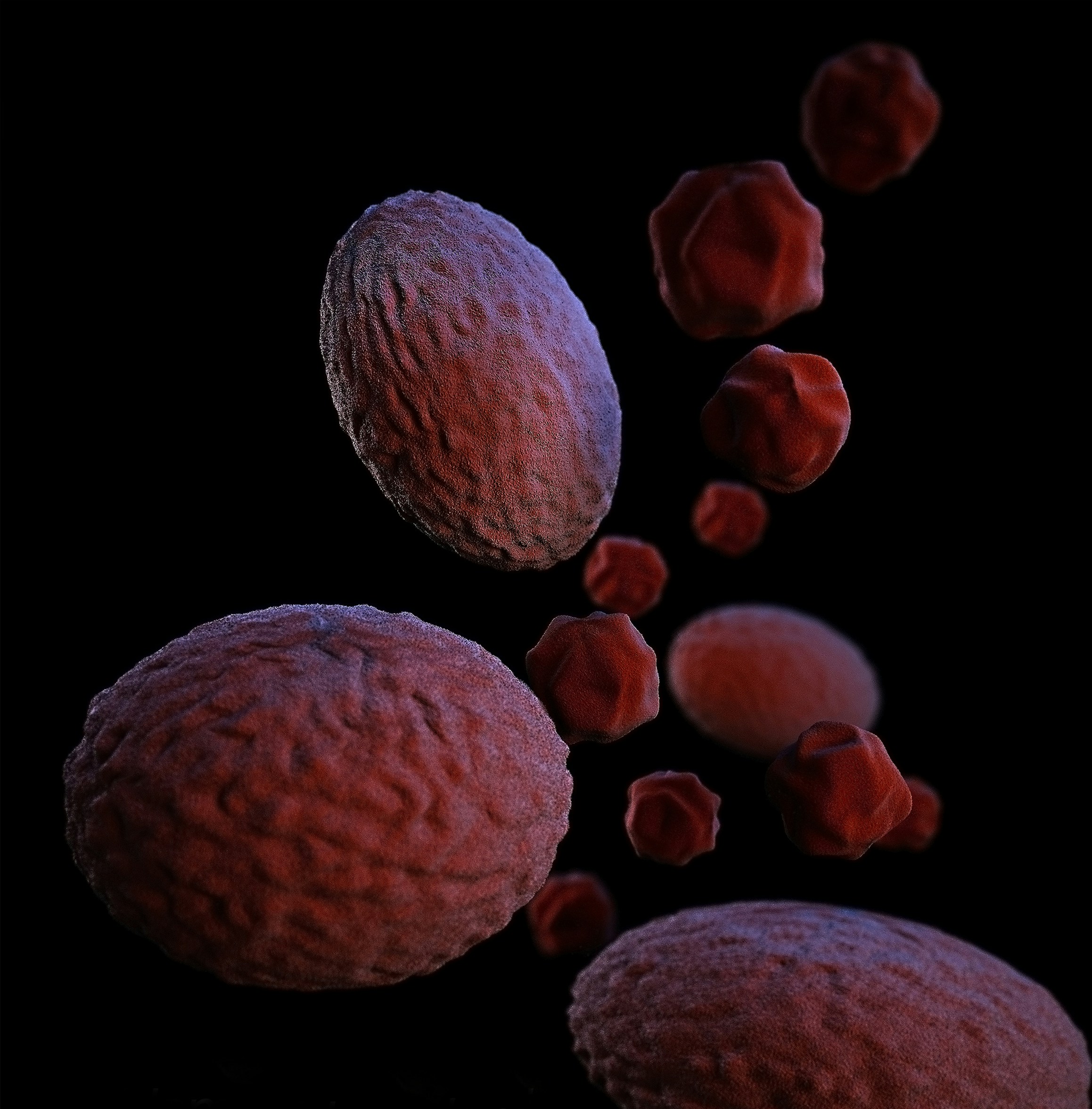
Sandhoff Disease is a condition that can occur in anyone, regardless of their background, ethnicity, or family history. It is caused by a specific genetic mutation that leads to the harmful accumulation of certain substances in the nerve cells of the brain and spinal cord. These substances, which are normally broken down and removed, build up to toxic levels and disrupt the normal functioning of these vital areas of the nervous system.
As a result, individuals with Sandhoff Disease often experience a range of severe symptoms that can include muscle weakness, motor skill regression, intellectual disability, and seizures. The disease typically manifests in infancy or early childhood and, unfortunately, progresses rapidly. The impact on the affected individual and their family can be profound, as they navigate the challenges posed by this debilitating condition.
Understanding Sandhoff Disease is crucial not only for those who may be directly affected but also for the wider community. Raising awareness about this rare genetic disorder can help foster a supportive environment for families and encourage further research into potential treatments and therapies. By learning about Sandhoff Disease, we can all contribute to a more informed and compassionate society.
What Causes Sandhoff Disease?
Sandhoff disease is rooted in our genetic makeup, specifically in the genes that control the production of certain vital enzymes. These enzymes, known as hexosaminidase A and hexosaminidase B, play a critical role in breaking down fatty substances called GM2 gangliosides within our cells. When there is a deficiency or malfunction in these enzymes, GM2 gangliosides accumulate, leading to the progressive damage of nerve cells in the brain and spinal cord.
The genetic basis for this enzyme deficiency lies in mutations in the HEXB gene. Each person inherits two copies of this gene, one from each parent. For Sandhoff disease to manifest, a child must inherit two defective copies of the HEXB gene, one from each parent. This mode of inheritance is known as autosomal recessive. If both parents are carriers, there is a 25% chance with each pregnancy that the child will have Sandhoff disease.
To simplify understanding, remember the mnemonic: ‘Faulty genes, fatty build-up, that’s the way Sandhoff shows up.’ This phrase encapsulates how defective genes lead to the harmful accumulation of fatty substances in the body, which in turn causes the symptoms of Sandhoff disease. Essentially, the absence of functional enzymes due to genetic mutations prevents the body from properly managing these fatty substances, leading to their toxic build-up.
Understanding the genetic cause of Sandhoff disease highlights the importance of genetic counseling and testing, particularly for families with a history of the condition. Early diagnosis through genetic testing can provide crucial information for managing the disease and planning for the future. Moreover, ongoing research into gene therapy and other treatments offers hope for more effective interventions in the years to come.
Symptoms to Watch Out For
Sandhoff Disease is a rare genetic disorder that primarily affects the central nervous system. Recognizing its symptoms early can be crucial for managing the condition. One of the hallmark symptoms is muscle weakness. This can manifest as difficulty in lifting objects, frequent falls, or trouble climbing stairs. Over time, this weakness becomes more pronounced, affecting the ability to perform everyday tasks.
Loss of motor skills is another significant symptom. Children who once could walk, sit up, or grasp objects may begin to lose these abilities. This regression can be distressing for both the child and their caregivers. For instance, a child who previously enjoyed building with blocks might suddenly struggle to pick them up or even hold them.
Vision problems are also common in individuals with Sandhoff Disease. This can range from mild blurriness to severe vision impairment. Parents might notice their child squinting often, struggling to see objects clearly, or becoming unusually clumsy, bumping into furniture or walls.
In addition to these main symptoms, other signs can include exaggerated startle reactions to loud noises, developmental delays, and an enlarged liver or spleen. These symptoms collectively paint a picture of the disease’s progression and can help in early diagnosis.
To make it easier to remember these symptoms, here’s a simple rhyme:
Weak muscles, vision blur,Movements slow, these signs infer.
This rhyme encapsulates the core symptoms of Sandhoff Disease, making it easier for both healthcare providers and families to recall the critical signs to watch out for. Early detection and intervention can significantly impact the quality of life for those affected by this challenging condition.
Diagnosing Sandhoff Disease
Diagnosing Sandhoff Disease involves a series of genetic tests and clinical evaluations. Doctors begin by assessing the patient’s symptoms, which may include progressive muscle weakness, loss of motor skills, and developmental delays. These symptoms raise suspicion and prompt further investigation.
Genetic testing is the cornerstone of diagnosing Sandhoff Disease. These tests analyze the patient’s DNA for mutations in the HEXB gene, which are indicative of the condition. A simple blood sample is typically all that is needed to conduct these tests. “Genes tell the tale, tests don’t fail, doctors find the trail” serves as a memorable way to understand the diagnostic journey.
In practical terms, consider the example of a family noticing their child’s developmental delays and muscle weakness. Concerned, they visit a pediatrician who refers them to a genetic specialist. The specialist conducts a thorough clinical evaluation and orders a genetic test. The results reveal mutations in the HEXB gene, confirming the diagnosis of Sandhoff Disease. This diagnosis enables the family to understand the condition and seek appropriate care and support.
Beyond genetic testing, imaging studies such as MRI scans may be employed to detect brain abnormalities associated with Sandhoff Disease. Additionally, enzyme assays can be conducted to measure the activity of β-hexosaminidase A and B enzymes. Reduced activity of these enzymes further supports the diagnosis.
Early and accurate diagnosis is crucial for managing Sandhoff Disease effectively. It allows healthcare providers to offer the best possible care plans and enables families to access necessary resources and support systems. By understanding the diagnostic process, families can navigate this challenging journey with greater clarity and confidence.
Living with Sandhoff Disease: Practical Tips
Living with Sandhoff Disease can be challenging, but with the right approach, families can create a supportive and nurturing environment for their loved ones. Supportive care, physical therapy, and community support play crucial roles in managing the symptoms and enhancing the quality of life for individuals with Sandhoff Disease.
Supportive care encompasses a variety of services, including medical management, nutritional support, and respiratory care. Regular consultations with healthcare professionals ensure that the individual’s needs are continuously monitored and addressed. It is essential to establish a routine for administering medications, as consistency can significantly impact the individual’s overall well-being.
Physical therapy is another vital component of care. Engaging in regular physical activity, tailored to the individual’s capabilities, helps maintain muscle strength, improve mobility, and reduce the risk of complications. A physical therapist can design a personalized exercise program that promotes physical and emotional health. Simple activities like stretching, gentle exercises, and hydrotherapy can make a substantial difference.
Community support is invaluable for both the individual with Sandhoff Disease and their family. Joining support groups or online communities can provide emotional relief and practical advice from others who understand the journey. Sharing experiences and coping strategies fosters a sense of solidarity and reduces feelings of isolation.
To illustrate, consider the Johnson family, who adapted their home to better care for their daughter, Emily, diagnosed with Sandhoff Disease. They installed ramps for easier wheelchair access and designated a therapy room with soft mats and equipment for Emily’s exercises. The family also set up a weekly schedule that includes physical therapy sessions, medical check-ups, and time for community group meetings. They live by the mantra: ‘Support and care, families share, therapies and love, rise above,’ which reminds them of the collective effort required to support Emily.
By integrating these practical tips, families can create a structured and loving environment that supports the well-being of their loved ones with Sandhoff Disease. Through consistent care, therapy, and community engagement, it is possible to navigate the challenges and focus on the positive aspects of the journey.
There’s a light at the end of the tunnel for those affected by Sandhoff Disease, thanks to ongoing research and advancements in medical science. Scientists around the world are diligently working to unravel the complexities of this rare genetic disorder, aiming to develop effective treatments that can significantly improve the quality of life for patients.
One of the most promising areas of research is gene therapy. This innovative approach involves correcting the underlying genetic defect that causes Sandhoff Disease. By introducing functional copies of the defective gene into patients’ cells, researchers hope to restore normal enzyme activity, which is crucial for breaking down certain fats in the body. Early trials have shown encouraging results, suggesting that gene therapy could one day offer a long-term solution for managing the disease.
Another exciting avenue of research is enzyme replacement therapy (ERT). This method focuses on supplementing the missing or deficient enzyme in patients with Sandhoff Disease. ERT has already shown success in treating other lysosomal storage disorders, and scientists are optimistic that it could be adapted for Sandhoff Disease. This approach could potentially alleviate some of the debilitating symptoms and slow the progression of the disease.
Additionally, researchers are exploring the potential of small molecule drugs that can cross the blood-brain barrier and target the central nervous system where Sandhoff Disease causes significant damage. These drugs aim to reduce the accumulation of harmful substances in the brain, thereby protecting nerve cells and preserving cognitive function.
Collaborative efforts and increased funding are also critical in driving forward the research on Sandhoff Disease. Organizations and foundations dedicated to rare genetic disorders are providing essential support, fostering a sense of community and hope among affected families. These collective efforts are paving the way for breakthroughs that were once considered unattainable.
While there is still much work to be done, the progress made thus far is a testament to the resilience and determination of the scientific community. As research continues to advance, there is renewed hope that effective treatments, and perhaps even a cure, will become a reality for those living with Sandhoff Disease.