Introduction to Pompe Disease
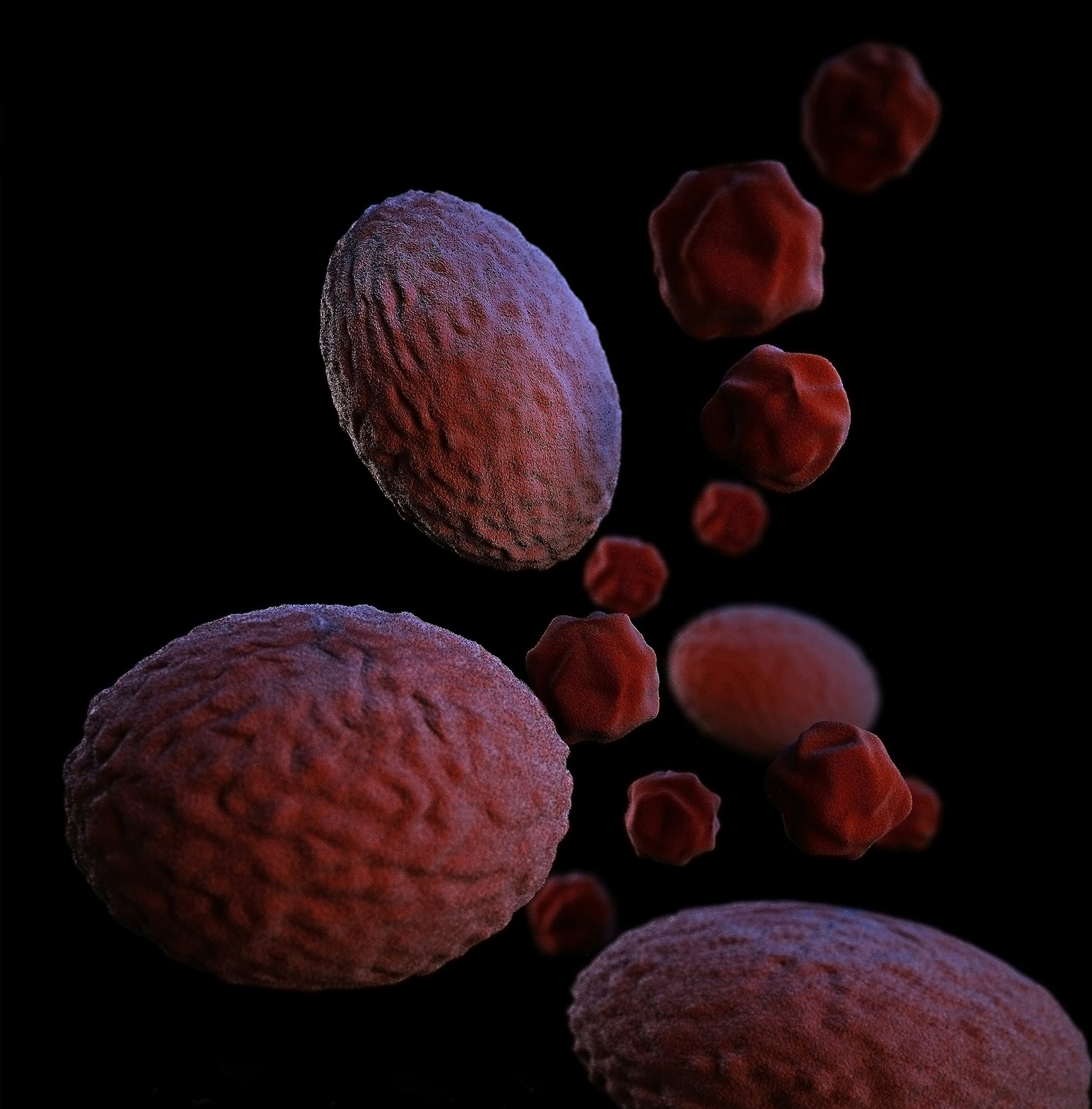
Pompe disease is a rare genetic disorder that significantly impacts muscle and nerve cells. At its core, the disease is caused by the buildup of a complex sugar known as glycogen. Typically, our bodies break down glycogen into glucose, which is then used for energy. However, in individuals with Pompe disease, this process is disrupted due to a lack of a specific enzyme, leading to the accumulation of glycogen within cells.
Imagine Anna, a young girl who loves playing soccer but finds herself unusually tired and weak after just a few minutes on the field. Despite her enthusiasm, her muscles don’t seem to cooperate, and she often experiences difficulty breathing. After numerous visits to doctors, Anna is diagnosed with Pompe disease. This diagnosis explains her symptoms, as the excess glycogen in her muscle cells prevents them from functioning correctly.
Pompe disease manifests in various ways, depending on the age of onset and the severity of enzyme deficiency. In infants, it can cause severe muscle weakness, heart problems, and respiratory issues. In contrast, adults may experience progressive muscle weakness, particularly in the legs and trunk, making everyday activities increasingly challenging.
Understanding Pompe disease is crucial not only for those diagnosed but also for their families, friends, and caregivers. By recognizing the fundamental aspects of the disorder, we can better support those affected and foster a more inclusive environment. As we delve deeper into this guide, we will explore the causes, symptoms, diagnosis, and available treatments for Pompe disease, providing a comprehensive overview to aid in comprehension and awareness.
How Pompe Disease Affects the Body
Pompe disease is a complex condition with far-reaching effects on the body. Primarily, it targets the muscles and respiratory system, leading to a range of symptoms that can significantly impact daily life. To make understanding these symptoms easier, remember the mnemonic ‘POMPE’:
Poor muscle tone, Overload of glycogen, Muscle weakness, Pulmonary issues, and Enlarged heart.
Firstly, poor muscle tone is a hallmark of Pompe disease. This manifests as difficulty in maintaining posture, which often leads to problems with walking and standing. Affected individuals may find themselves stumbling or unable to support their own weight for extended periods. This is due to the overload of glycogen in the muscles, a direct consequence of the deficiency of the enzyme acid alpha-glucosidase. The inability to break down glycogen effectively results in its accumulation, which disrupts normal muscle function.
Muscle weakness is another prominent symptom. Over time, the muscles lose their strength and endurance, making everyday tasks such as climbing stairs or lifting objects increasingly challenging. This muscle weakness can be particularly pronounced in the legs and hips, contributing to the aforementioned difficulties in mobility.
Respiratory, or pulmonary, issues are also common. The muscles involved in breathing can weaken, leading to shortness of breath, especially during physical activity. In more severe cases, individuals may require mechanical ventilation to assist with breathing. These pulmonary complications highlight the importance of regular monitoring and early intervention to manage respiratory health.
Additionally, Pompe disease can cause an enlarged heart, a condition known as cardiomegaly. This can lead to further complications, including heart failure, which underscores the need for comprehensive cardiac care in affected individuals.
To help remember these key symptoms, consider this simple rhyme:
“Poor muscles and glycogen’s plight,Weakness in limbs, breathing’s fight.
Heart grows big, a daunting sight,Pompe’s effects are not light.”
This mnemonic and rhyme aim to simplify the complexities of Pompe disease, making it easier to understand and recall the primary ways it affects the body.
Diagnosing Pompe Disease
Diagnosing Pompe disease involves a series of steps that help doctors to identify the condition accurately. Imagine a patient, Jane, who visits her doctor due to persistent muscle weakness and fatigue. Her doctor suspects Pompe disease and begins the diagnostic process.
The first step is usually a blood test. This test measures the levels of a specific enzyme called acid alpha-glucosidase (GAA). In individuals with Pompe disease, the levels of GAA are significantly lower than normal. Jane’s blood test results reveal low GAA levels, indicating a potential case of Pompe disease.
To confirm the initial findings, the doctor orders a genetic test. This test examines Jane’s DNA for mutations in the GAA gene, which are responsible for the disease. Genetic testing is highly accurate and can definitively diagnose Pompe disease. Jane’s test results show mutations in the GAA gene, confirming the diagnosis.
In some cases, doctors may also recommend a muscle biopsy. This involves taking a small sample of muscle tissue to examine under a microscope. The biopsy can reveal characteristic signs of Pompe disease, such as the accumulation of glycogen in muscle cells. For Jane, the muscle biopsy further supports the diagnosis, showing the typical glycogen buildup.
Throughout the diagnostic process, it’s vital for doctors to consider the patient’s symptoms, medical history, and test results collectively. By using these diagnostic tools, doctors can accurately diagnose Pompe disease and provide the necessary care and treatment for patients like Jane.
Understanding these diagnostic steps helps demystify the process and ensures that individuals are informed about how Pompe disease is identified and confirmed.
Treatment and Management
Pompe disease, a rare genetic disorder, requires a multifaceted approach for effective treatment and management. One of the cornerstone treatments is Enzyme Replacement Therapy (ERT). This therapy is akin to adding a missing ingredient in a recipe; just as a cake won’t rise without baking powder, the body struggles without specific enzymes. ERT introduces the necessary enzyme into the patient’s system, helping mitigate the disease’s progression and alleviate symptoms. Myozyme (alglucosidase alfa) is a widely used enzyme replacement that has shown significant improvements in muscle function and respiratory health in many patients.
Real-life examples illustrate the profound impact of ERT on individuals with Pompe disease. For instance, a young child diagnosed early and started on ERT has shown remarkable developmental milestones, such as improved motor skills and enhanced respiratory function. Similarly, an adult patient reported a notable increase in energy levels and a reduction in muscle pain, allowing them to resume daily activities that were previously challenging.
In addition to ERT, supportive care plays a vital role in managing Pompe disease. Physical therapy is essential to maintain muscle strength and flexibility, preventing the deterioration that can occur with the disease. Respiratory support, including non-invasive ventilation, is often necessary as the disease can affect respiratory muscles, leading to difficulties in breathing. These supportive measures, combined with ERT, provide a comprehensive management strategy that significantly enhances the quality of life for patients.
Moreover, dietary modifications and regular monitoring by healthcare professionals are crucial components of the management plan. Ensuring adequate nutrition and addressing potential complications early can help in maintaining overall health and well-being. The collaborative effort of a multidisciplinary team, including geneticists, neurologists, and physical therapists, ensures that patients receive the holistic care they need to navigate the complexities of Pompe disease.
“`html
Living with Pompe Disease: Practical Tips
Living with Pompe disease requires thoughtful planning and adjustments to daily routines. Establishing a consistent schedule can help manage symptoms and improve quality of life. For instance, incorporating regular rest periods throughout the day can help conserve energy and prevent fatigue. It’s essential to listen to your body and not overexert yourself.
Diet plays a critical role in managing Pompe disease. A balanced diet rich in proteins, vitamins, and minerals can support muscle strength and overall health. Consulting with a nutritionist can help create a meal plan tailored to individual needs. Hydration is equally important, so make sure to drink plenty of water throughout the day.
Exercise, although challenging, is vital for maintaining muscle function. Low-impact activities such as swimming, yoga, or walking can be beneficial. Always consult with a healthcare provider before starting any exercise regimen to ensure it is safe and appropriate for your condition. Physical therapy can also provide personalized exercises that target specific muscle groups affected by Pompe disease.
Support networks are invaluable for those living with Pompe disease. Connecting with others who understand the challenges can provide emotional support and practical advice. Online forums, local support groups, and social media communities can be great resources. Building a strong support system, including family and friends, can make a significant difference in managing daily life.
Consider the story of the Martinez family, who have been living with Pompe disease for several years. They attribute their positive outlook to a well-structured routine, a nutritious diet, and regular physical activity. “Every day may not be good, but there’s something good in every day,” says Mrs. Martinez, highlighting the importance of finding joy in small victories.
Remember, while living with Pompe disease presents unique challenges, it is possible to lead a fulfilling life with the right strategies and support. As the saying goes, “Tough times never last, but tough people do.” Stay resilient and proactive in managing your health.
“`
Raising Awareness and Support
Raising awareness about Pompe disease is critical in ensuring that patients and their families receive the support they need. Pompe disease, a rare genetic disorder, often goes undiagnosed or misdiagnosed, leading to delayed treatment and support. Increased public awareness can lead to earlier detection, better treatment outcomes, and more comprehensive support systems for those affected. It is essential for communities, healthcare providers, and policymakers to collaborate in spreading knowledge about this condition.
One effective way to support patients and their families is by joining support groups. These groups provide a platform for sharing experiences, advice, and emotional support. They also offer access to valuable resources, such as educational materials and information about the latest treatments and clinical trials. For instance, organizations like the Acid Maltase Deficiency Association (AMDA) play a crucial role in connecting patients with the necessary support and information.
Participating in awareness campaigns is another impactful way to support the Pompe disease community. These campaigns often involve events, social media drives, and educational workshops that aim to inform the public and healthcare professionals about the condition. A notable example is the International Pompe Day, held annually on April 15. This global event unites patients, families, advocates, and researchers to raise awareness and funds for research. The success of such campaigns highlights the power of community support in making a difference.
To truly make a lasting impact, readers are encouraged to get involved in these awareness efforts. Whether by participating in local events, sharing information on social media, or supporting relevant organizations, every action counts. By contributing to these initiatives, individuals can help ensure that those affected by Pompe disease receive the recognition and support they deserve.