Introduction to Cori’s Disease
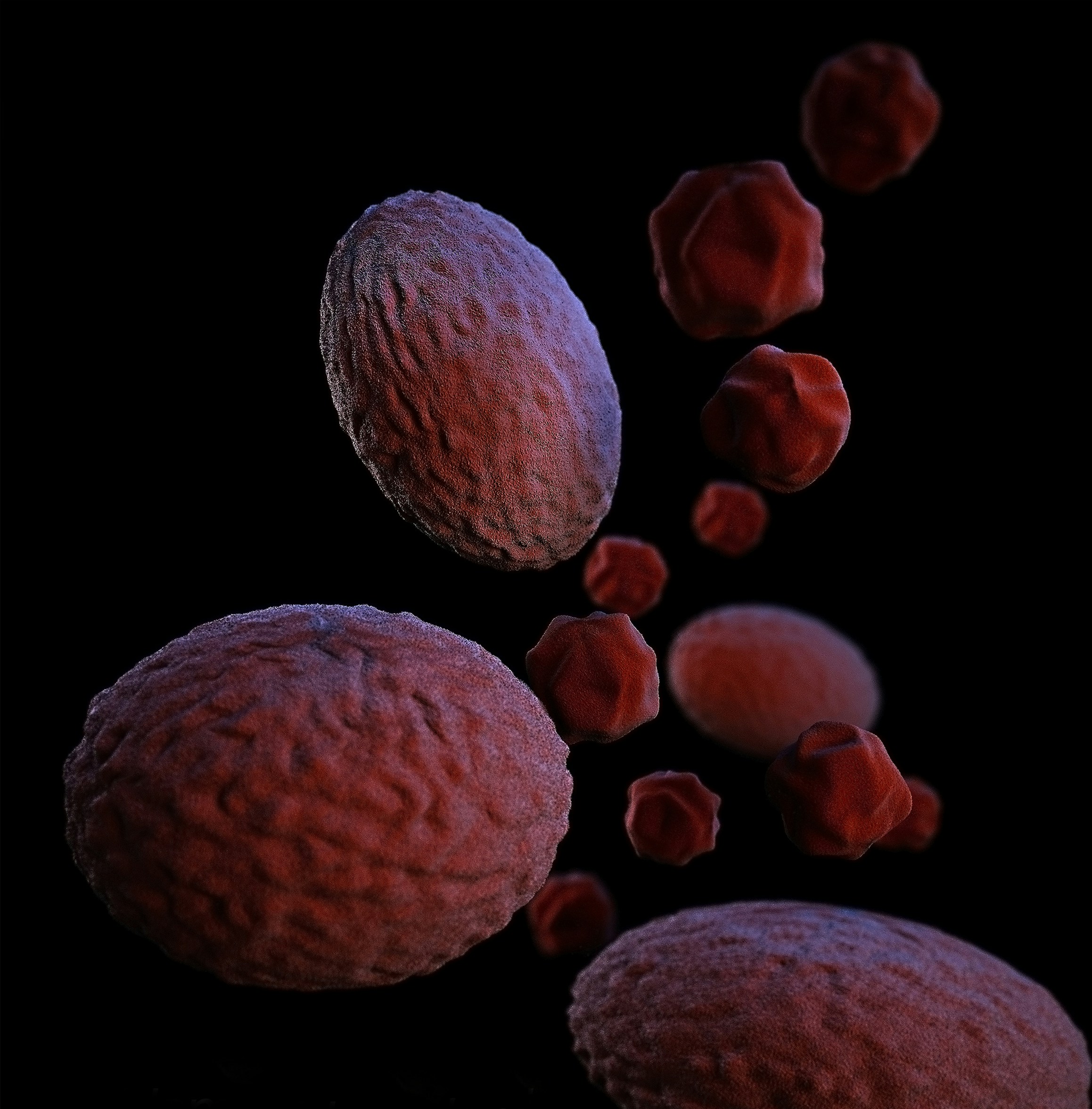
Cori’s Disease, also known scientifically as Glycogen Storage Disease Type III, is a rare genetic disorder that affects the body’s ability to break down glycogen. Glycogen is a form of stored sugar that our bodies use for energy. In a healthy individual, enzymes break down glycogen into glucose, which is then used by our cells for energy. However, in individuals with Cori’s Disease, a specific enzyme called debranching enzyme is either missing or not functioning properly. This leads to an abnormal accumulation of glycogen in the liver and muscles, causing a range of health issues.
To understand how Cori’s Disease affects daily life, let’s consider a typical day for a child living with this condition. Imagine a young boy named Alex. Alex wakes up feeling unusually tired, despite having slept for a full night. His energy levels are low because his body struggles to convert glycogen into glucose. Breakfast time can be stressful; Alex must follow a strict diet to manage his blood sugar levels, which means frequent meals and snacks to prevent hypoglycemia (low blood sugar).
During school, Alex might find it difficult to concentrate and keep up with his classmates. Physical education classes present another challenge, as his muscles fatigue quickly and he may experience muscle cramps or even weakness. Teachers and peers need to be aware of his condition to provide the necessary support and understanding.
In the afternoon, Alex has a playdate, but he must be cautious about overexerting himself. His parents constantly monitor his activity levels and ensure he has access to quick sources of sugar, like glucose tablets, in case of an emergency. Dinner includes a carefully planned meal to balance his energy needs, followed by a bedtime routine that often involves medication and sometimes even a nighttime feeding to maintain steady glucose levels overnight.
Through this day in the life of Alex, we see that while Cori’s Disease presents significant challenges, with proper management and understanding, individuals can lead fulfilling lives. This introduction sets the stage for a deeper exploration into the complexities of Cori’s Disease, its symptoms, diagnosis, and treatment options, which will be covered in the following sections.
Understanding the Basics: The Role of Glycogen
In simple terms, glycogen is like a battery that stores energy for our bodies to use when needed. Imagine that every time you eat, your body converts some of the food into this special form of energy storage. This stored energy, known as glycogen, is kept primarily in your liver and muscles. When your body requires energy between meals or during physical activity, it breaks down the glycogen into glucose, which is then used as fuel.
Now, consider a scenario where this ‘battery’ doesn’t work correctly—this is essentially what happens in Cori’s Disease. Also known as Glycogen Storage Disease Type III, Cori’s Disease is a disorder that affects the body’s ability to break down glycogen. The issue stems from a deficiency in an enzyme called debranching enzyme, which is crucial for breaking down glycogen into glucose. Without this enzyme functioning properly, glycogen accumulates in the liver and muscles, leading to various symptoms such as low blood sugar, muscle weakness, and an enlarged liver.
To help remember these key points, think of the mnemonic “Good Dogs Get Bad Bones.” This stands for Glycogen, Debranching enzyme, Glucose, Breakdown, and Blocked—highlighting the essential elements of what goes wrong in Cori’s Disease. Another catchy rhyme could be: “Glycogen’s our energy store; if broken, we feel weak and sore.” By keeping these simple analogies and mnemonics in mind, understanding the complex nature of glycogen and its malfunction in Cori’s Disease becomes a bit easier.
This malfunctioning ‘battery’ not only affects energy levels but can also lead to more severe health issues if not managed properly. Therefore, recognizing the role of glycogen and the impact of its breakdown is crucial in understanding Cori’s Disease and its effects on the body.
Symptoms and Diagnosis
Cori’s Disease, also known as Glycogen Storage Disease Type III, presents a range of symptoms that can be challenging to identify without proper medical knowledge. One of the most common symptoms is low blood sugar, or hypoglycemia, which can result in dizziness, fatigue, and confusion. Imagine a child who frequently feels weak and tired, struggling to maintain normal energy levels despite regular meals. This could be a sign of Cori’s Disease.
Another notable symptom is muscle weakness. Patients may experience difficulty with everyday tasks, such as climbing stairs or lifting objects. This muscle weakness can be particularly noticeable during periods of physical exertion. Picture a young athlete who suddenly finds it hard to keep up with peers during sports activities or playtime; such a scenario might indicate underlying muscle issues related to Cori’s Disease.
Additionally, an enlarged liver, known as hepatomegaly, is a hallmark of Cori’s Disease. Parents might notice that their child’s abdomen appears unusually swollen or firm. This enlargement occurs because the liver stores excess glycogen, which the body cannot properly break down. Regular pediatric check-ups can help in early detection of such physical changes.
Doctors diagnose Cori’s Disease through a series of steps. Initial physical exams can reveal signs like an enlarged liver or muscle weakness. Blood tests are crucial to measure glucose levels and liver enzymes, which often show abnormalities in affected individuals. Genetic testing provides a definitive diagnosis by identifying mutations in the AGL gene responsible for the disease.
To make it easier to remember these symptoms and diagnostic methods, consider this simple rhyme:
Low blood sugar makes you dizzy,Muscle weakness makes tasks busy,
An enlarged liver, big and round,Blood tests and genes, diagnosis found.
Recognizing these signs early and consulting healthcare professionals can lead to timely diagnosis and management of Cori’s Disease, improving quality of life for affected individuals.
Living with Cori’s Disease: Management and Treatment
Managing Cori’s Disease, also known as Glycogen Storage Disease Type III, involves a multifaceted approach that includes dietary modifications, regular meal schedules, and, in some cases, medication. The primary goal is to maintain stable blood glucose levels and prevent hypoglycemia, a common complication of the disease. This requires a carefully planned regimen tailored to each patient’s individual needs.
One of the most critical aspects of managing Cori’s Disease is adhering to a special diet. Patients often need to consume frequent, small meals rich in complex carbohydrates to ensure a steady release of glucose. This dietary strategy helps in maintaining energy levels and preventing the severe drops in blood sugar that can lead to dangerous health episodes. For instance, a typical day for a child with Cori’s Disease might include meals every three to four hours, with snacks in between to keep blood sugar levels stable.
In addition to diet, some patients might require medications to manage symptoms or address specific complications associated with Cori’s Disease. Medications such as cornstarch supplements can provide a slow-release form of glucose, further aiding in blood sugar management. However, the necessity and type of medication vary from case to case, highlighting the importance of personalized medical care.
To illustrate, consider a family with a young child diagnosed with Cori’s Disease. The family might collaborate with a dietitian to develop a meal plan that includes frequent, nutrient-rich snacks. They might also schedule activities around meal times to ensure the child has consistent energy levels. School teachers and caregivers would be informed of the child’s needs, ensuring a supportive environment outside the home.
The role of a dedicated healthcare team cannot be overstated. Regular consultations with a pediatrician, endocrinologist, and dietitian are crucial for ongoing management. This team provides invaluable support, helping to adjust dietary plans, monitor health status, and administer necessary treatments. They also offer guidance and education to the family, empowering them to manage the disease effectively.
In conclusion, living with Cori’s Disease requires a comprehensive and adaptive approach. Through careful dietary management, potential medication, and the unwavering support of a healthcare team, patients can lead healthy and active lives despite the challenges of the disease.
Support Systems and Resources
Dealing with Cori’s Disease can be an overwhelming experience for individuals and their families. Fortunately, a variety of support systems and resources are available to help navigate this challenging journey. These resources can provide not only critical information but also emotional support and a sense of community.
One of the most valuable resources for families dealing with Cori’s Disease is support groups. These groups often consist of individuals and families who are either directly or indirectly affected by the disease. They offer a platform for sharing experiences, coping strategies, and practical advice. For instance, the Glycogen Storage Disease Program at the University of Florida hosts support groups that can connect families with others facing similar challenges, fostering a sense of solidarity and mutual understanding.
Online communities also play a crucial role in providing support for those affected by Cori’s Disease. Websites such as RareConnect and Facebook groups dedicated to Glycogen Storage Diseases enable individuals to share their stories, ask questions, and receive encouragement from others worldwide. These virtual communities are especially beneficial for those who may not have access to local support groups, ensuring that no one has to face their journey alone.
In addition to support groups and online communities, numerous organizations offer valuable resources for individuals with Cori’s Disease. For example, the United Mitochondrial Disease Foundation (UMDF) and the Association for Glycogen Storage Disease (AGSD) provide comprehensive information on disease management, research updates, and advocacy opportunities. These organizations often host conferences, webinars, and workshops that can be instrumental in educating families and healthcare providers about the latest advancements in the field.
Practical examples of how these resources can make a difference include connecting families with expert healthcare providers, offering guidance on managing daily challenges, and providing emotional support through shared experiences. Access to these support systems and resources can significantly improve the quality of life for individuals with Cori’s Disease and their loved ones, helping them to feel more empowered and informed.
Hope and Future Research
As our understanding of Cori’s Disease continues to evolve, the future looks increasingly promising. Researchers around the globe are diligently working to uncover new treatments and potential cures. Current studies are exploring innovative approaches, such as gene therapy and enzyme replacement therapy, which aim to address the root causes of this metabolic disorder.
Gene therapy, in particular, holds significant promise. By correcting the genetic mutations responsible for Cori’s Disease, this cutting-edge technique could potentially offer a long-term solution for those affected. Early-stage clinical trials have already shown encouraging results, paving the way for more extensive research and development.
Enzyme replacement therapy (ERT) is another area of active investigation. This treatment involves supplementing the deficient enzyme in patients with Cori’s Disease to restore normal metabolic function. While still in the experimental phase, ERT has demonstrated potential in preclinical models, bringing hope to patients and their families.
In addition to these advanced therapies, ongoing research is also focused on improving diagnostic methods and enhancing supportive care. Early and accurate diagnosis is crucial for effective management of Cori’s Disease, and advancements in genetic testing are making it possible to identify the condition earlier than ever before. Supportive care, including dietary management and regular monitoring, remains essential for maintaining quality of life for individuals with this condition.
Collectively, these efforts signify a brighter future for those living with Cori’s Disease. The dedication of scientists, healthcare professionals, and advocacy groups is driving progress toward more effective treatments and, ultimately, a cure.
With every study and trial, we move closer to a day when Cori’s Disease is no longer a burden. As we look to the horizon, let us take heart in the strides being made and the collective hope that fuels this journey.
“In the realm of science, we find our way, Bringing hope for a brighter day.With each step forward, we near the cure,A future free from Cori’s Disease, we shall ensure.”