Introduction to Cystic Fibrosis
Imagine a young boy named Timmy who loves playing outside but often finds himself struggling to catch his breath. He frequently experiences lung infections that make it difficult for him to engage in the activities he enjoys. Timmy’s condition is known as Cystic Fibrosis (CF), a genetic disorder that primarily affects the lungs and digestive system. This disorder is more than just an occasional inconvenience; it significantly impacts his daily life and overall health.
Cystic Fibrosis is caused by mutations in the CFTR (Cystic Fibrosis Transmembrane Conductance Regulator) gene. This gene plays a critical role in regulating the movement of salt (sodium chloride, or NaCl) and water in and out of the cells. In individuals with CF, these mutations lead to the production of a defective CFTR protein, which disrupts the normal balance of salt and water.
To understand how this disruption occurs, think of the CFTR protein as a gatekeeper that controls the flow of salt and water, much like how a functional sink drain regulates water flow. In a healthy individual, this gatekeeper ensures that mucus in the lungs and digestive system remains thin and slippery, allowing it to be easily cleared out. However, in someone with CF, the defective CFTR protein acts like a clogged sink drain. This causes the mucus to become thick and sticky, obstructing the airways and making it difficult to breathe. This thick mucus also creates an environment that is prone to bacterial infections, leading to the frequent lung infections Timmy experiences.
Understanding the role of the CFTR gene and its impact on the movement of salt and water is crucial in grasping why Cystic Fibrosis manifests the way it does. It not only affects the respiratory system but also has significant implications for the digestive system, leading to various complications that require ongoing medical attention. Through Timmy’s story, we gain a relatable perspective on the challenges faced by individuals with CF and the importance of ongoing research and treatment efforts.
The Role of Mucin in Cystic Fibrosis
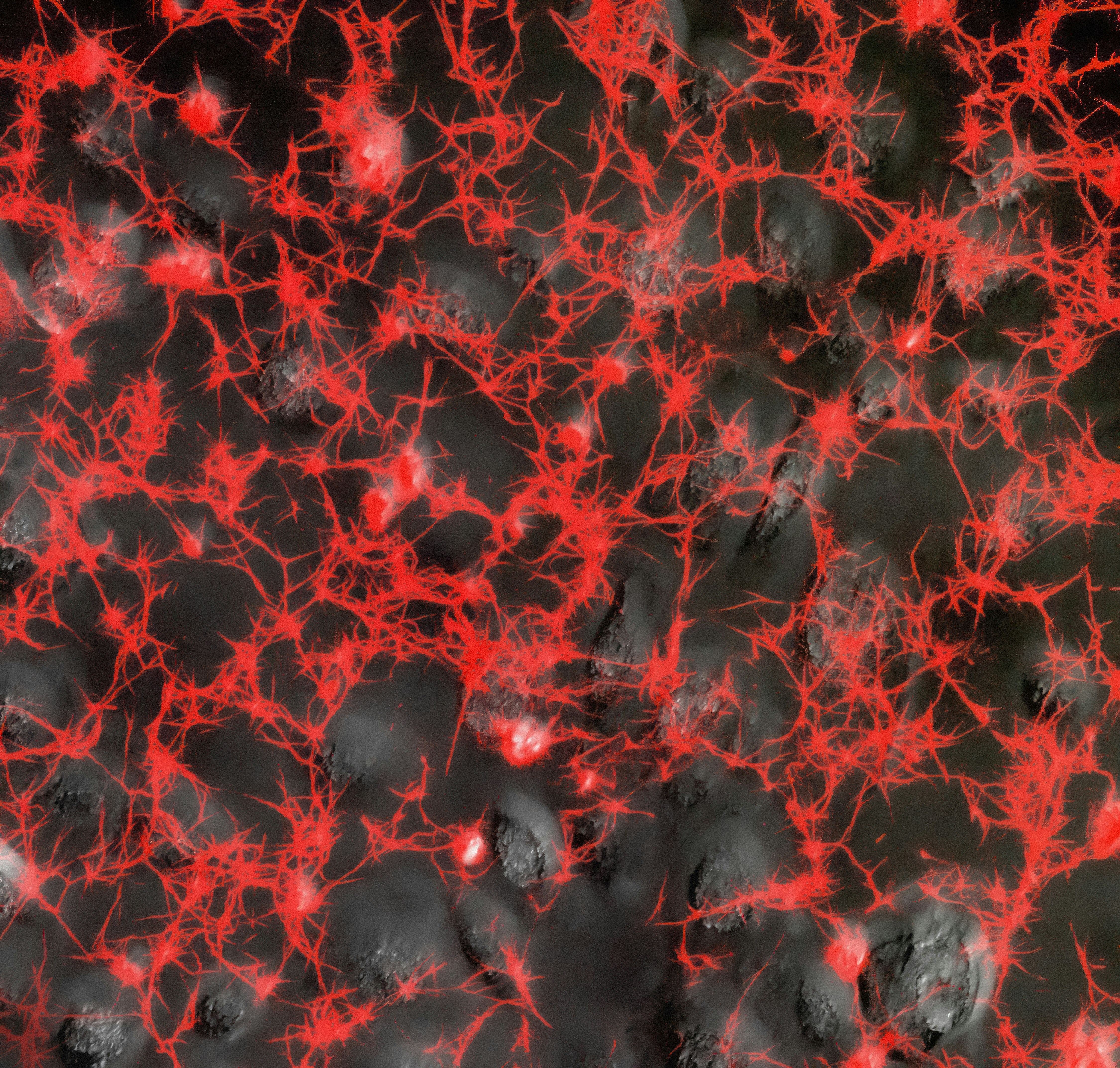
Mucin, mucin, sticky and slick, helps our bodies fight off the sick. Produced by the body to keep the lungs and digestive system moist, mucin plays a crucial role in maintaining our health. This slippery substance provides a protective layer, ensuring that airways and digestive tracts remain lubricated. However, in the case of cystic fibrosis (CF), mucin behaves differently due to a defective CFTR gene.
In individuals with CF, mucin becomes excessively thick and sticky. This is because the faulty CFTR gene disrupts the balance of salt and water on the surface of the cells, leading to a thicker mucus. Imagine trying to drink a thick milkshake through a narrow straw; that’s how tough it becomes for someone like Timmy, who has CF, to breathe. The dense mucus clogs airways, making it difficult to clear out bacteria and other pathogens. As a result, frequent infections and respiratory complications become a common struggle.
This overly viscous mucin doesn’t just affect the lungs; it also impacts the digestive system. The thick mucus can obstruct the pancreatic ducts, preventing digestive enzymes from reaching the intestines. Consequently, individuals with CF may suffer from malnutrition and poor growth because their bodies cannot properly digest and absorb nutrients from food.
Understanding the role of mucin in cystic fibrosis highlights the importance of maintaining proper mucus consistency for respiratory and digestive health. Effective management of CF often includes therapies aimed at thinning the mucus, making it easier to expel and reducing the risk of infections. By addressing the root cause—the abnormal mucus consistency—we can improve the quality of life for those living with cystic fibrosis.
The Importance of NaCl (Salt) Balance
NaCl, more commonly known as table salt, plays a critical role in maintaining the proper balance of fluids within our bodies. This balance is crucial for the optimal functioning of our cells, tissues, and organs. To help remember this essential function, consider the mnemonic ‘Salt Helps Cells Stay Happy’ (SHCSH). When salt is correctly balanced, cells can efficiently manage fluid levels, thereby ensuring that they remain healthy and functional.
However, in individuals with cystic fibrosis (CF), the movement of salt in and out of cells is significantly disrupted. This disruption primarily occurs due to a malfunction in the CFTR (Cystic Fibrosis Transmembrane Conductance Regulator) protein. The CFTR protein is responsible for regulating the flow of chloride ions, which are a component of salt, across cell membranes. When this regulation is impaired, it leads to an imbalance in salt and water transport.
To better understand how this imbalance affects the body, imagine making a soup. Normally, you would add a precise amount of salt to achieve the perfect consistency. If you add too much salt, the soup becomes too thick and hard to stir. Similarly, in CF, an excess of salt inside the cells makes the mucus on the surface of organs, especially the lungs, abnormally thick and sticky. This thick mucus obstructs airways and creates a breeding ground for harmful bacteria, leading to persistent infections and inflammation.
Thus, maintaining the proper salt balance is crucial for preventing the thickening of mucus and ensuring that cells can perform their functions efficiently. Understanding the role of NaCl in cystic fibrosis helps us appreciate the challenges faced by individuals with this condition and underscores the importance of developing treatments that can restore the balance of salt and fluids in their bodies.
The CFTR Gene and Its Function
The CFTR gene can be likened to a skilled traffic cop, directing the flow of salt and water across cell membranes. In this analogy, the smooth movement of ions resembles the orderly flow of vehicles through a well-regulated intersection. The CFTR protein, produced by the CFTR gene, acts as a channel that allows chloride ions to move in and out of cells, maintaining the right balance of salt and water on the surfaces of organs like the lungs and pancreas.
Imagine now that this traffic cop is suddenly replaced by a malfunctioning traffic light. When the light malfunctions, it causes a traffic jam because vehicles can’t move as they should. Similarly, mutations in the CFTR gene disrupt its normal function, leading to a kind of ‘traffic jam’ at the cellular level. The result is a build-up of thick, sticky mucus instead of the thin, free-flowing mucus that would normally help protect and lubricate our organs.
This faulty traffic light scenario illustrates how a broken CFTR gene can lead to cystic fibrosis (CF). In CF patients, the defective CFTR protein can’t adequately regulate the movement of chloride ions. Consequently, water can’t follow chloride ions into the mucus lining, causing mucus to become abnormally thick and sticky. This thick mucus can clog airways and create a breeding ground for bacteria, leading to frequent lung infections and other complications.
In a healthy system, the CFTR gene ensures that chloride ions smoothly pass through cell membranes, keeping mucus at the right consistency to trap and expel pathogens and debris. However, with a defective CFTR gene, this delicate balance is disrupted, leading to the hallmark symptoms of cystic fibrosis. By understanding the CFTR gene’s role as a traffic cop, we can better appreciate how essential it is in maintaining cellular harmony and how its malfunction leads directly to the complications seen in CF.
Real-Life Impact of Cystic Fibrosis
Cystic fibrosis (CF) is not just a clinical diagnosis; it profoundly affects the daily lives of individuals and their families. Take Timmy, a 12-year-old boy with CF, as an example. Timmy’s day begins with a series of breathing treatments and chest physiotherapy, designed to loosen the thick mucus in his lungs. This routine is essential but time-consuming, often making him late for school and extracurricular activities.
Frequent hospital visits are another reality for Timmy. Infections are common due to the thick mucus that traps bacteria, leading to frequent admissions for intravenous antibiotics. These hospital stays disrupt his schooling and social life, causing him to fall behind in class and miss out on time with friends. His family also feels the strain, both emotionally and financially, as they juggle medical bills and time off work to care for him.
Dietary restrictions add another layer of complexity to Timmy’s life. CF affects the digestive system, making it difficult for him to absorb nutrients. As a result, he needs a high-calorie, high-fat diet supplemented with vitamins and pancreatic enzymes. Meals are not just about eating but also about carefully measuring and monitoring his intake, which can be exhausting for both Timmy and his caregivers.
The emotional toll is immense. Timmy often feels isolated and different from his peers, who don’t have to worry about daily treatments and hospital visits. His parents grapple with constant anxiety over his health, balancing hope and fear with each new symptom or hospital admission. The weight of living with CF can be likened to carrying a heavy backpack all day—it’s exhausting and makes every aspect of life more challenging.
In essence, the impact of cystic fibrosis extends far beyond the physical symptoms. It affects every facet of life, requiring immense strength, resilience, and support from both the individual and their loved ones. Understanding these challenges helps us appreciate the courage of those living with CF and underscores the importance of ongoing research and support in this field.
Current Treatments and Research
Cystic fibrosis (CF) management revolves around three critical pillars: medications, chest physiotherapy, and dietary supplements, conveniently remembered as ‘Meds, Moves, Meals’ (MMM). Each of these components plays a vital role in alleviating symptoms and improving the quality of life for individuals with CF.
Medications include a range of drugs designed to tackle various aspects of CF. Mucolytics, such as dornase alfa, help thin the mucus in the lungs, making it easier to expel. Antibiotics are crucial for treating and preventing lung infections, while CFTR modulators like ivacaftor and lumacaftor work to correct the underlying defect in the CFTR protein. Anti-inflammatory drugs are also used to reduce lung inflammation.
Moves refers to chest physiotherapy, a cornerstone of CF treatment. This form of therapy involves techniques like percussion, postural drainage, and the use of devices such as oscillating positive expiratory pressure (PEP) to help clear mucus from the airways. Physical exercise is also encouraged to enhance respiratory function and overall health.
Meals highlights the importance of nutrition in CF care. People with CF often experience malabsorption due to pancreatic insufficiency. Enzyme supplements are therefore essential to aid digestion and nutrient absorption. High-calorie, high-fat diets are recommended to ensure sufficient energy intake. Additionally, vitamins and minerals, particularly fat-soluble vitamins (A, D, E, and K), are supplemented to address deficiencies.
Ongoing research in CF is akin to a lighthouse guiding ships to safety, offering hope for more effective treatments and a potential cure. Gene therapy is at the forefront of this research, with the aim to correct the defective CFTR gene. Advances in CRISPR technology and viral vector delivery systems are showing promising results in preclinical trials. Other innovative approaches include developing more effective CFTR modulators and exploring stem cell therapy to repair damaged lung tissue.
In conclusion, the current landscape of CF treatment and research offers a hopeful future, with continuous advancements paving the way for better management and potential cures. By embracing the ‘Meds, Moves, Meals’ approach and keeping an eye on emerging therapies, individuals with CF can look forward to improved health outcomes and enhanced quality of life.