Introduction to Diabetic Ketoacidosis (DKA)
Imagine a young woman, Sarah, who has been living with diabetes for several years. One evening, she starts feeling extremely thirsty, nauseous, and finds it difficult to breathe. Despite drinking water, her symptoms worsen, and she eventually collapses. When rushed to the hospital, doctors diagnose her with Diabetic Ketoacidosis (DKA), a serious and potentially life-threatening complication of diabetes.
Diabetic Ketoacidosis, or DKA, occurs when the body begins to break down fats at an accelerated rate, producing acidic ketone bodies that accumulate in the blood. This process is akin to a car engine running out of fuel; when the fuel (glucose) is insufficient, the engine (body) starts to malfunction, causing a cascade of problems. In a healthy body, insulin helps glucose enter cells to be used for energy. However, in individuals with diabetes, particularly Type 1 diabetes, the lack of insulin leads to elevated blood sugar levels and an inability to utilize glucose for energy.
As the body desperately seeks alternative fuel sources, it begins to break down fat, resulting in the production of ketones. While ketones can serve as an emergency energy source, their accumulation leads to a dangerous state of metabolic acidosis. The blood becomes increasingly acidic, disrupting normal physiological functions and ultimately posing serious health risks if not treated promptly.
DKA is not just a minor hiccup in the body’s functioning; it is a medical emergency that requires immediate intervention. Symptoms such as excessive thirst, frequent urination, fatigue, nausea, vomiting, and abdominal pain can rapidly escalate to more severe conditions like difficulty breathing, confusion, and even loss of consciousness. Understanding DKA’s causes and mechanisms is crucial for both healthcare providers and individuals managing diabetes, as early recognition and treatment can be life-saving.
Causes of Diabetic Ketoacidosis
Diabetic Ketoacidosis (DKA) is a serious complication of diabetes that occurs when the body starts breaking down fats at an excessive rate, leading to a buildup of acids in the bloodstream. Understanding the causes of DKA is crucial for both prevention and effective management. A helpful mnemonic to remember the primary causes is ‘MISS,’ which stands for Missed insulin, Infection, Stress, and Sickness.
Firstly, Missed insulin doses are a common cause of DKA. Insulin is essential for regulating blood sugar levels, and missing a dose can lead to a rapid rise in blood glucose. For example, a person with diabetes who forgets their insulin shot may experience a significant increase in blood sugar, triggering the onset of DKA.
Secondly, Infection is another significant trigger. Infections, such as urinary tract infections or pneumonia, can cause the body to release stress hormones like cortisol and adrenaline, which counteract the effects of insulin. This can lead to elevated blood sugar levels and potentially DKA. For instance, a simple cold or flu can escalate into a severe condition requiring medical attention if blood sugar levels are not adequately controlled.
Stress also plays a crucial role in the development of DKA. Emotional or physical stress can increase blood sugar levels by prompting the release of stress hormones. Situations such as surgery, trauma, or even emotional upheaval can lead to a significant rise in blood glucose, increasing the risk of DKA.
Lastly, general Sickness that affects the body’s ability to manage blood sugar can precipitate DKA. Conditions like gastroenteritis, which affect nutrient absorption, or chronic illnesses that impact overall health, can destabilize blood sugar levels. For example, a person with diabetes experiencing severe vomiting may find it challenging to maintain their usual insulin regimen, resulting in uncontrolled blood sugar and the potential for DKA.
By recognizing the ‘MISS’ causes of DKA—Missed insulin, Infection, Stress, and Sickness—individuals with diabetes and their caregivers can better anticipate and prevent this life-threatening complication.
Pathophysiology: What Happens Inside the Body?
When insulin’s gone, the body’s in need, it breaks down fat at lightning speed. The cells crave glucose, but it’s locked away, so the body finds another way. It turns to fat, a secondary source, breaking it down with urgent force. This process, called lipolysis, begins, and soon ketones are flooding in.
Ketones rise, the blood turns sour, it’s an emergency, hour by hour. These ketones, though small, are potent and strong, making the blood’s pH go wrong. Acidosis sets in, creating a mess, as the body’s systems start to stress. The kidneys work hard, trying to cope, flushing out ketones, a glimmer of hope.
But as ketones build, the danger’s clear, dehydration and imbalance draw near. Electrolytes tumble, potassium falls, the heart and muscles heed the call. Breathing becomes deep, a desperate gasp, Kussmaul’s respiration takes the grasp. To blow off CO2 and counter the pH, the body struggles in this race.
The brain, too, feels the dire strain, as confusion and fatigue reign. Consciousness can ebb away, in this metabolic disarray. As glucose levels skyrocket high, hyperglycemia adds to the sky. The osmolality of blood goes up, causing the body’s cells to erupt.
So, from insulin’s lack to fat’s breakdown, the body fights, but starts to drown. Ketones rise, the blood turns acidic, the pathophysiology becomes quite specific. Understanding these steps, it’s clear to see, why DKA is an emergency.
Recognizing the Symptoms: When to Seek Help
Diabetic Ketoacidosis (DKA) manifests through a variety of symptoms that can be easily mistaken for other conditions. Therefore, recognizing these “red flags” is critical to ensuring timely medical intervention. Common symptoms of DKA include excessive thirst, frequent urination, nausea, abdominal pain, and confusion. These warning signs are the body’s way of signaling that it is in distress and requires immediate attention.
To aid in the identification of these symptoms, the mnemonic ‘THIRST’ can be particularly useful:
Thirst: One of the earliest signs of DKA is an unquenchable thirst. This is due to the high levels of glucose in the blood that draw water out of the cells, causing dehydration.
Heavy Breathing: As the body attempts to expel excess acids, breathing may become labored and deep, known as Kussmaul respirations.
Increased Urination: Frequent urination is a direct result of the kidneys trying to eliminate the excess glucose from the bloodstream.
Stomach Pain: Abdominal pain and discomfort are common as the digestive system is affected by the high levels of ketones.
Tiredness: Extreme fatigue and weakness occur because the body is unable to effectively use glucose for energy.
Recognizing these symptoms early can be lifesaving. If you or someone you know exhibits any combination of these signs, it is imperative to seek medical assistance immediately. DKA is a medical emergency that can escalate rapidly, leading to severe complications such as cerebral edema, arrhythmias, and even death if not treated promptly.
In summary, understanding and identifying the symptoms of DKA using the ‘THIRST’ mnemonic can greatly aid in early detection and timely medical intervention. Always err on the side of caution and consult a healthcare professional if you suspect DKA.
Treatment: Steps to Manage Diabetic Ketoacidosis
Diabetic ketoacidosis (DKA) requires immediate and meticulous intervention, akin to executing a well-coordinated rescue mission. The first step in managing DKA is to promptly administer insulin. This vital hormone helps to lower high blood sugar levels and curtail the production of ketones, which are harmful acids that accumulate in the bloodstream during DKA. Administering insulin is akin to stabilizing the foundation of a collapsing structure; it is the primary and most urgent action required to restore balance.
Simultaneously, rehydration through intravenous fluids is critical. DKA often results in severe dehydration due to excessive urination caused by high blood glucose levels. Providing fluids helps to replenish lost moisture, stabilize blood pressure, and improve circulation. It’s like filling a parched desert with much-needed water, restoring the body’s fluid balance and ensuring that essential organs receive adequate blood flow.
Following the initial stabilization, attention shifts to electrolyte replacement. DKA can cause significant imbalances in essential electrolytes such as potassium, sodium, and chloride. Correcting these imbalances is crucial to prevent complications such as cardiac arrhythmias and muscle weakness. Monitoring and adjusting electrolyte levels is akin to fine-tuning an instrument to ensure that all components function harmoniously.
Continuous monitoring in a hospital setting is the next step. Medical professionals will frequently check blood glucose levels, ketone levels, and overall metabolic status to ensure that the treatment is effective. This phase of treatment is comparable to a vigilant security detail, continuously assessing the situation to prevent any unforeseen complications.
In severe cases, additional interventions may be required, such as bicarbonate therapy to address severe acidosis or advanced supportive care in an intensive care unit. Each step in the DKA treatment process is essential, much like the coordinated efforts of a rescue team, ensuring that the patient emerges from the crisis stabilized and on the path to recovery.
Prevention: How to Keep Diabetic Ketoacidosis at Bay
Preventing Diabetic Ketoacidosis (DKA) is essential for individuals managing diabetes. Effective prevention strategies can significantly reduce the risk of this serious complication. The mnemonic ‘TRACK’ provides a simple yet comprehensive guide to help remember key prevention measures: Test regularly, Routine care, Avoid triggers, Communicate with your doctor, and Keep emergency contacts.
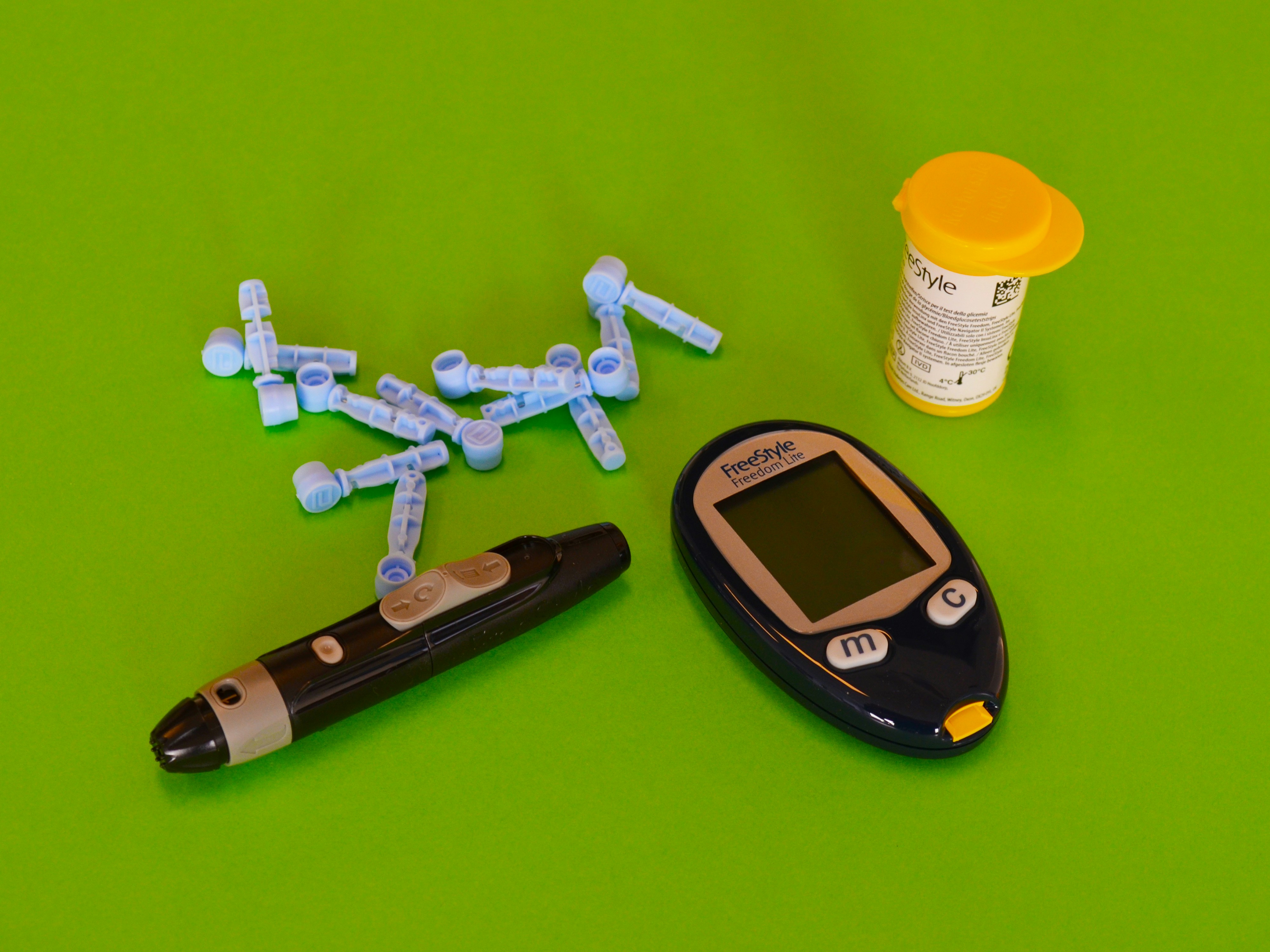
Test Regularly: Regular monitoring of blood sugar levels is fundamental in preventing DKA. Frequent testing helps in identifying any abnormal fluctuations early, allowing for timely intervention. Use a reliable glucose meter and maintain a log of your readings. This practice enables you to notice trends and adjust your management plan accordingly.
Routine Care: Adhering to your prescribed insulin therapy or oral medication regimen is crucial. Skipping doses or not following the recommended schedule can lead to uncontrolled blood sugar levels, increasing the risk of DKA. Combine this with a balanced diet and regular physical activity to maintain optimal glucose levels. Routine check-ups with your healthcare provider are also vital to monitor your condition and make necessary adjustments to your treatment plan.
Avoid Triggers: Certain factors such as infections, stress, and improper diet can trigger episodes of high blood sugar, leading to DKA. Practice good hygiene, manage stress through relaxation techniques, and adhere to a diabetes-friendly diet. Stay informed about potential triggers and take proactive measures to avoid them.
Communicate with Your Doctor: Open and regular communication with your healthcare provider is essential. Discuss any changes in your symptoms, challenges in managing your diabetes, or concerns about your treatment plan. Your doctor can provide valuable advice, adjust your medications, and help you develop a more effective management strategy.
Keep Emergency Contacts: Ensure you have a list of emergency contacts, including your healthcare provider and local emergency services. In the event of a DKA episode, having these contacts readily available can expedite medical assistance and potentially save your life.
Incorporating these prevention strategies into your daily routine can significantly reduce the risk of Diabetic Ketoacidosis. By following the ‘TRACK’ mnemonic and creating a personalized action plan, you can effectively manage your diabetes and maintain better overall health.