Introduction to Hypoketotic Hypoglycemia in MCAD
Hypoketotic hypoglycemia is a condition characterized by low blood sugar levels without the expected increase in ketone bodies, which are substances produced when the body breaks down fat for energy. This condition is particularly significant when linked to Medium-Chain Acyl-CoA Dehydrogenase (MCAD) deficiency, a genetic disorder that impairs the body’s ability to convert certain fats into energy, especially during periods of fasting or increased energy demands.
To understand how MCAD deficiency leads to hypoketotic hypoglycemia, envision the body as a car that can run on two types of fuel: gasoline (glucose) and diesel (fat). In individuals with MCAD deficiency, the engine that processes diesel is faulty. So, when gasoline runs low, the car can’t switch to diesel efficiently. Similarly, people with MCAD deficiency struggle to break down medium-chain fatty acids into ketones, which would normally serve as an alternative energy source when glucose is scarce.
This condition primarily affects infants and young children, but it can also persist into adulthood. It often becomes apparent during periods when the body’s glucose reserves are depleted, such as overnight fasting, illness, or prolonged physical activity. Symptoms may include lethargy, seizures, and even coma if not promptly treated. Early diagnosis and management are crucial to prevent severe complications.
Understanding hypoketotic hypoglycemia in the context of MCAD deficiency is vital for several reasons. Firstly, it enables affected individuals and their families to recognize the signs and symptoms early, ensuring timely medical intervention. Secondly, it highlights the importance of genetic screening, particularly in newborns, to identify those at risk. Lastly, awareness can lead to better dietary and lifestyle adjustments that help manage the condition effectively, thereby improving the quality of life for those affected.
A Real-Life Scenario: Meet Tommy
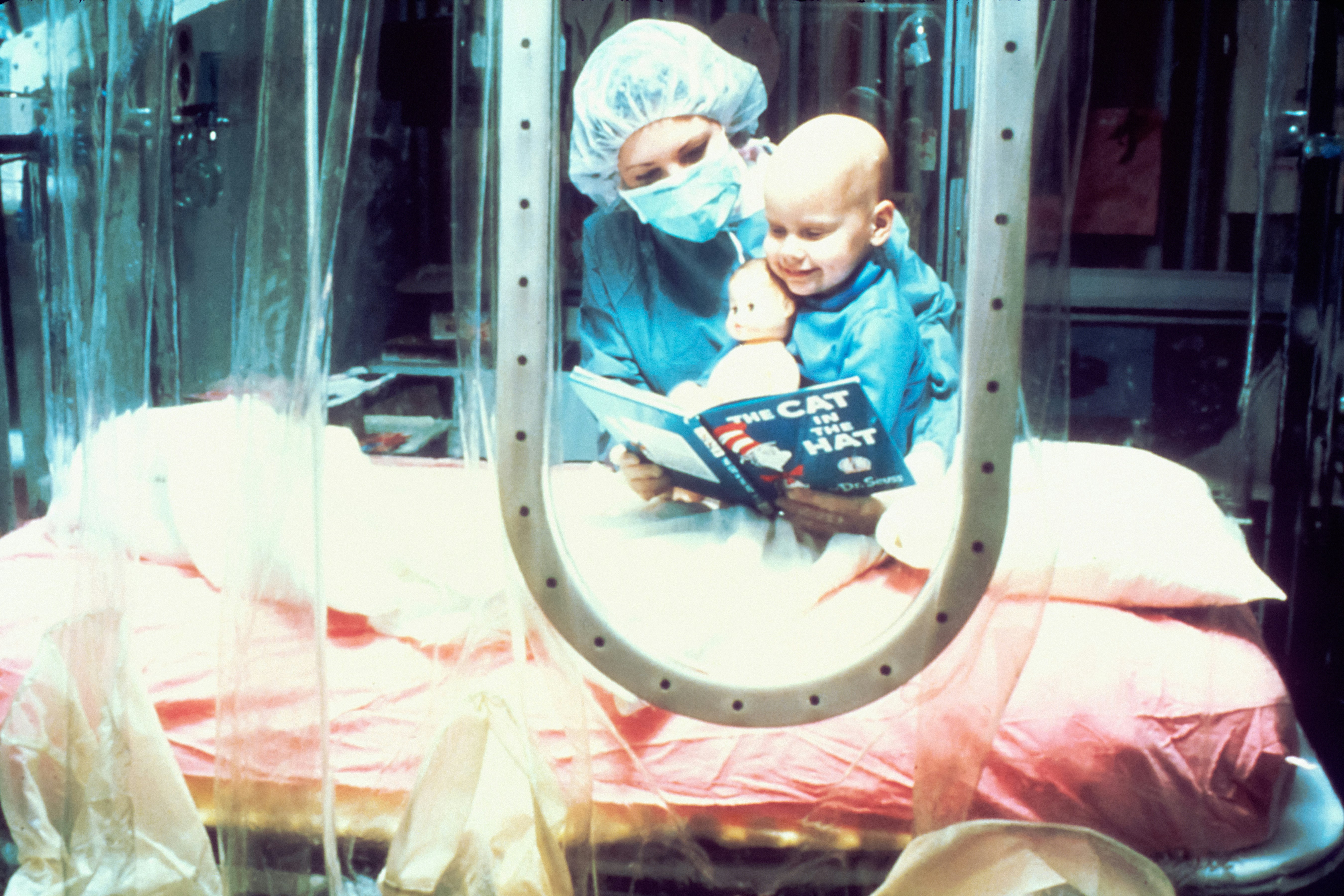
Meet Tommy, a vibrant six-year-old with an adventurous spirit. Despite his enthusiasm, Tommy has Medium-Chain Acyl-CoA Dehydrogenase (MCAD) deficiency, a metabolic disorder that affects his body’s ability to convert certain fats into energy. This condition makes Tommy prone to hypoketotic hypoglycemia, a type of low blood sugar that occurs without the production of ketones, which are usually generated during fat breakdown.
A typical day for Tommy begins like any other child’s—he wakes up, eager to play and learn. However, his parents are always vigilant about his meal schedule. Tommy needs to eat frequent, balanced meals and snacks to maintain his blood sugar levels. Skipping even one meal can leave him feeling weak and dizzy, hallmark symptoms of hypoketotic hypoglycemia. For instance, if Tommy misses his mid-morning snack during school, he might become lethargic, irritable, and find it hard to concentrate on his lessons. This is because his body struggles to produce enough energy from fats, leading to a dangerous drop in blood sugar levels.
To manage his condition, Tommy carries a small pack of snacks wherever he goes—granola bars, fruit slices, or cheese sticks. These snacks are not just a convenience; they are a crucial part of his daily routine. His teachers are informed about his condition and are trained to recognize the early signs of hypoglycemia. If Tommy appears unusually tired or confused, they know it’s time for a quick snack break.
Tommy’s parents have also adapted their lifestyle to ensure his well-being. Family outings and activities are planned around his meal times. They have learned to prepare high-carbohydrate meals that provide a steady energy release. Simple adjustments, such as carrying a cooler with perishable snacks during trips, have become second nature.
Through these practical measures, Tommy leads a fulfilling life, navigating the challenges of MCAD deficiency with the support and understanding of those around him. Regular meals and snacks are not just dietary recommendations; they are essential for Tommy’s health and well-being, allowing him to enjoy his childhood with fewer disruptions.
Mnemonic Devices to Remember Key Facts
Mnemonic devices can be invaluable tools for recalling critical information about hypoketotic hypoglycemia in MCAD, especially given the complexity of the condition. One effective mnemonic to remember the core issue is “FAT” – standing for “Fatty Acid Trouble.” This reminds us that hypoketotic hypoglycemia in MCAD is fundamentally related to problems with fat metabolism, as the body’s ability to break down fatty acids is impaired.
Another helpful mnemonic for remembering the primary symptoms is “WEAK.” Here’s the breakdown:
- Weakness
- Energy deficit
- Appetite loss
- Ketone absence
These symptoms highlight the energy crisis resulting from the body’s inability to utilize fatty acids effectively, leading to low energy levels and the absence of ketones.
For understanding the treatment approach, consider the mnemonic “FUEL,” which emphasizes the critical aspects of managing the condition:
- Frequent meals
- Use of carbohydrates
- Emergency glucose
- Lifestyle adjustments
This mnemonic underscores the importance of maintaining stable blood glucose levels through regular meals, carbohydrate intake, and emergency glucose administration, along with necessary lifestyle changes.
Lastly, for prevention strategies, “SAFE” serves as a simple reminder:
- Sugar monitoring
- Avoid fasting
- Family education
- Early intervention
These key actions help manage the condition effectively and prevent hypoglycemic episodes by ensuring consistent blood sugar levels, avoiding prolonged fasting, educating family members, and acting swiftly when symptoms arise.
A Poem to Simplify the Concept
When fats are stuck, and sugar’s low,
Tommy feels it head to toe.
His energy drops, like a setting sun,
Hypoketotic hypoglycemia isn’t fun.
MCAD, a tricky name,
Means his body can’t play the fuel game.
Fats can’t turn to sugar’s might,
So Tommy’s strength takes flight.
In the cells where magic’s brewed,
Enzymes work to make our food.
But in MCAD, the gears don’t turn,
Leaving Tommy’s tummy to churn.
When he skips a meal or plays too long,
Tommy’s energy feels all wrong.
Blood sugar dips, he feels so weak,
It’s hypoketotic hypoglycemia he seeks.
With care and snacks, he’ll be okay,
His family helps him every day.
MCAD is tough, but knowledge is power,
To keep Tommy strong, hour by hour.
Practical Tips for Managing MCAD
Managing MCAD (Medium-Chain Acyl-CoA Dehydrogenase Deficiency) on a daily basis requires thoughtful planning and vigilance. Below are some practical tips that can help in managing this condition effectively.
Meal Planning
One of the most crucial aspects of managing MCAD is diligent meal planning. Consuming regular meals and snacks throughout the day helps maintain stable blood sugar levels. Focus on a balanced diet that includes a variety of nutrients. Incorporate complex carbohydrates, proteins, and healthy fats into every meal. Foods like whole grains, lean meats, vegetables, and fruits are excellent choices. Avoid prolonged fasting; instead, aim to eat small meals every 3 to 4 hours.
Snacks
Always have snacks on hand to prevent hypoglycemia. Suitable snacks include fruit slices, cheese sticks, whole grain crackers, and yogurt. These options provide a good mix of carbohydrates and proteins, which can help sustain energy levels. For convenience, consider preparing snack packs that are easy to carry when on the go.
Emergency Preparedness
In case of an emergency, such as illness or an unexpected delay in meal times, it is essential to have a plan. Keep a stash of fast-acting carbohydrates like glucose tablets or juice boxes. Additionally, having an emergency medical kit with items like an emergency glucagon injection can be lifesaving. Make sure family members, friends, and caregivers are aware of the emergency plan and know how to use the emergency supplies.
Regular Check-Ups and Communication
Regular check-ups with healthcare providers are indispensable for managing MCAD. These visits allow for monitoring of metabolic levels and adjustments to management plans as needed. Open and frequent communication with your healthcare team ensures that any concerns or symptoms are promptly addressed. Don’t hesitate to discuss changes in appetite, energy levels, or any new symptoms with your doctor.
Incorporating these practical tips into daily life can significantly improve the management of MCAD, helping individuals lead healthier, more stable lives. Regular meal planning, smart snacking, emergency preparedness, and effective communication with healthcare providers are key components of managing this condition successfully.
Conclusion: Empowering Through Understanding
In this blog post, we delved into the critical aspects of hypoketotic hypoglycemia in MCAD, highlighting its causes, symptoms, diagnosis, and management. We explored how Medium-Chain Acyl-CoA Dehydrogenase deficiency disrupts the body’s ability to break down medium-chain fatty acids, resulting in episodes of hypoglycemia, particularly during fasting or illness. Recognizing the signs and symptoms, such as lethargy, vomiting, and seizures, is crucial for timely intervention.
Understanding the diagnostic process is essential, as early detection through newborn screening and specific blood tests can significantly improve the prognosis. Once diagnosed, managing hypoketotic hypoglycemia involves a combination of dietary modifications, regular monitoring, and emergency protocols to prevent and address hypoglycemic episodes.
Education and awareness play a pivotal role in empowering individuals and families affected by MCAD deficiency. By equipping themselves with the right knowledge and tools, they can effectively navigate the challenges posed by this condition. Healthcare providers, support groups, and educational resources are invaluable allies in this journey, offering guidance, support, and a sense of community.
Remember, you are not alone in facing hypoketotic hypoglycemia in MCAD. With the right information, proactive management strategies, and a supportive network, individuals and families can lead fulfilling lives despite the challenges. Always reach out to medical professionals and support groups for assistance and never hesitate to seek help when needed. Together, we can foster a better understanding and improve the quality of life for those living with MCAD deficiency.