What is Arteriosclerosis?
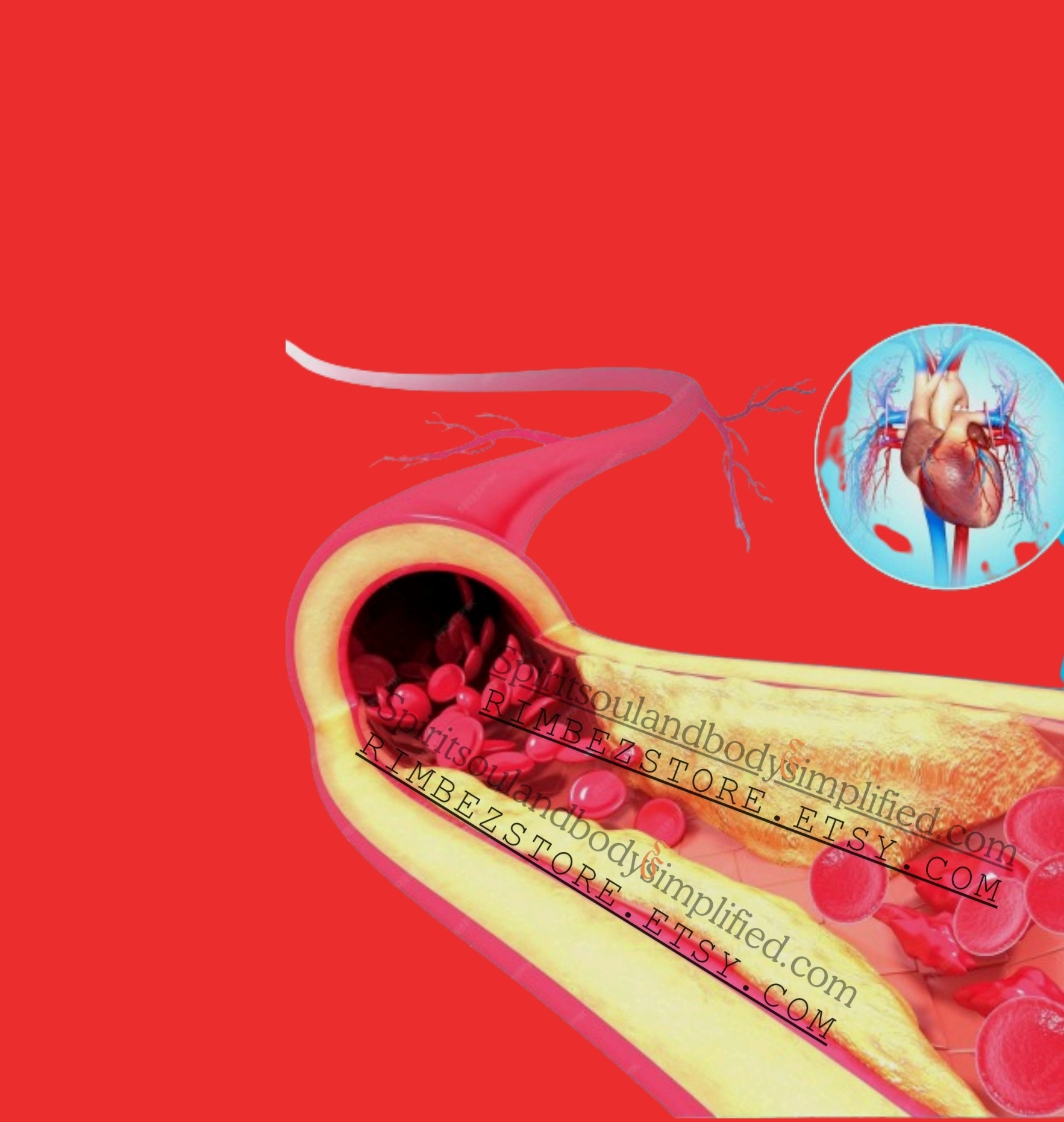
Arteriosclerosis is a term derived from the Greek words “arteria” meaning artery and “sclerosis” meaning hardening. Essentially, it refers to the hardening and thickening of the arterial walls. Think of your arteries as flexible straws that transport blood from your heart to the rest of your body. Over time, these straws can become stiff and thick, much like a garden hose left out in the sun, resulting in decreased elasticity. This stiffening process impedes the smooth flow of blood, akin to trying to drink a milkshake through a clogged straw.
Arteriosclerosis is a progressive condition that tends to be more prevalent with advancing age. As we grow older, the walls of our arteries naturally lose some of their elasticity, which can lead to this hardening. The condition can affect any artery in the body, including those in the heart, brain, and limbs, leading to various clinical implications depending on the affected area. For instance, if the arteries supplying the heart are impacted, it may result in coronary artery disease, while involvement of the brain’s arteries can lead to conditions such as stroke.
While arteriosclerosis is a common phenomenon, especially among the elderly, it is important to note that several risk factors can accelerate its onset. These factors include high blood pressure, high cholesterol levels, smoking, diabetes, and a sedentary lifestyle. On a cellular level, the process involves the accumulation of fatty deposits, cholesterol, and other substances within the arterial walls, forming plaques that contribute to the hardening and narrowing of the arteries.
Understanding arteriosclerosis is crucial because it serves as the underlying mechanism for many cardiovascular diseases. By recognizing this condition and its risk factors, individuals can take proactive steps to maintain arterial health and potentially mitigate the impacts of arteriosclerosis. This can include lifestyle modifications such as a balanced diet, regular physical activity, and smoking cessation, which collectively contribute to maintaining the flexibility and functionality of the arteries.
Signs and Symptoms
The signs and symptoms of arteriosclerosis can often be subtle and easily overlooked, yet they serve as crucial warning signals from the body. One useful mnemonic to remember these symptoms is ‘PEDS’—Pain, Exercise intolerance, Dizziness, and Shortness of breath. Each of these symptoms can manifest differently and might indicate varying levels of severity in the progression of arteriosclerosis.
Firstly, pain is a common symptom, often described as a pressing or squeezing sensation in the chest, akin to having an elephant sitting on one’s chest. This discomfort can radiate to the arms, neck, jaw, or back, making it challenging to pinpoint. This type of chest pain, known as angina, typically occurs when the heart muscle doesn’t get enough oxygen-rich blood, often due to narrowed or blocked arteries.
Secondly, exercise intolerance is another significant indicator. Individuals with arteriosclerosis might find themselves getting unusually tired or fatigued quickly during physical activities. Even routine tasks like walking up a flight of stairs can become exhausting. This diminished exercise capacity is a result of the heart struggling to pump blood efficiently through narrowed arteries.
Dizziness is another symptom that should not be ignored. It might occur due to reduced blood flow to the brain, leading to feelings of lightheadedness or even fainting spells. This symptom can be particularly alarming and might indicate that the brain is not receiving adequate oxygen.
Lastly, shortness of breath is a critical symptom, often arising when the heart cannot pump enough blood to meet the body’s needs. This can happen during physical exertion or even at rest, and it might be accompanied by a sensation of tightness in the chest or difficulty breathing.
While these symptoms can be indicative of arteriosclerosis, it’s important to note that some individuals may not experience any noticeable symptoms until a serious event, such as a heart attack or stroke, occurs. Hence, being vigilant and aware of these warning signs can be lifesaving, much like paying attention to a car’s check engine light.
Causes of Arteriosclerosis
Arteriosclerosis, a condition often likened to old, clogged pipes in a house, is influenced by several key factors. The mnemonic ‘FAST’—Fat, Age, Smoking, Tension—serves as a useful tool in understanding these contributing elements.
Firstly, the accumulation of fatty deposits within the artery walls, a process known as atherosclerosis, is a primary cause. These deposits, composed of cholesterol and other substances, gradually build up, narrowing the arteries and impeding blood flow. This can lead to serious cardiovascular complications, including heart attacks and strokes.
Secondly, aging plays a significant role in arteriosclerosis. As we age, our arteries naturally lose their elasticity, becoming stiffer and less able to expand and contract with each heartbeat. This reduced flexibility can make it more difficult for blood to flow smoothly through the arteries, increasing the risk of blockages and other cardiovascular issues.
Smoking is another major contributor. The harmful chemicals in cigarette smoke damage the inner lining of the arteries, known as the endothelium. This damage can lead to the formation of plaque, further narrowing the arteries and restricting blood flow. Additionally, smoking increases blood pressure and reduces the amount of oxygen that gets to the body’s tissues, compounding the problem.
Lastly, high blood pressure, or tension, places extra strain on the artery walls. This increased pressure can cause the arteries to thicken and harden over time, making them more susceptible to blockages. High blood pressure is often linked to other risk factors such as obesity, lack of physical activity, and poor diet, all of which can contribute to the development of arteriosclerosis.
In understanding these causes, individuals can take proactive steps to reduce their risk of arteriosclerosis, promoting better cardiovascular health and overall well-being.
Risk Factors
Arteriosclerosis is influenced by several key risk factors, which can be encapsulated by the mnemonic ‘SHADES’: Smoking, Hypertension, Age, Diabetes, Elevated cholesterol, and Sedentary lifestyle. Each of these factors contributes to the development and progression of arteriosclerosis, much like a garden overrun with weeds can stunt the growth of healthy plants.
Smoking is a major risk factor for arteriosclerosis. The chemicals in tobacco smoke damage the structure and function of blood vessels, leading to a buildup of plaque. This narrows the arteries and restricts blood flow, increasing the likelihood of heart attacks and strokes.
Hypertension, or high blood pressure, exerts extra force on the arterial walls, causing them to thicken and become less flexible. Over time, this can lead to the formation of plaques, further narrowing the arteries and impeding blood flow.
Age is another factor, as the risk of arteriosclerosis increases with advancing years. As individuals age, their arteries naturally lose some of their elasticity and are more prone to plaque accumulation, making older adults more susceptible to the condition.
Diabetes significantly elevates the risk of arteriosclerosis. High blood sugar levels can damage the inner lining of arteries, leading to plaque buildup. Diabetics are often also more likely to have other risk factors such as high blood pressure and high cholesterol, compounding their risk.
Elevated cholesterol levels, particularly low-density lipoprotein (LDL) cholesterol, can lead to the formation of plaques within the arteries. These plaques reduce the diameter of the arteries, restricting blood flow and increasing the risk of cardiovascular events.
Sedentary lifestyle is another contributing factor. Lack of regular physical activity can lead to weight gain, high blood pressure, and elevated cholesterol levels, all of which are risk factors for arteriosclerosis. Regular exercise helps maintain a healthy weight and promotes good cardiovascular health, reducing the risk of plaque buildup.
Understanding these risk factors is crucial in managing and preventing arteriosclerosis. By addressing these areas, individuals can significantly reduce their chances of developing this condition and maintain better overall cardiovascular health.
Complications
Arteriosclerosis, a condition characterized by the thickening and hardening of arterial walls, poses significant risks to overall health. To understand the potential complications, consider the mnemonic ‘CHESS’: Coronary artery disease, Heart attack, Stroke, and Silent ischemia. These complications can be life-threatening and warrant immediate attention.
Coronary artery disease (CAD) is a common consequence of arteriosclerosis. When the arteries supplying blood to the heart become narrowed or blocked, the heart muscle is deprived of essential oxygen and nutrients. This can lead to chest pain (angina) and, over time, weaken the heart’s function. If the blockage becomes complete, it may result in a heart attack, where parts of the heart muscle are damaged or die due to lack of oxygen.
Similarly, arteriosclerosis can result in a stroke, which occurs when the blood supply to part of the brain is interrupted or reduced. This can happen if an artery in the brain becomes blocked by a clot or bursts. The affected brain cells begin to die within minutes due to the lack of oxygen, leading to potential long-term neurological damage or death.
Silent ischemia is another severe consequence. Unlike a heart attack or stroke, silent ischemia may not exhibit noticeable symptoms, making it particularly dangerous. It occurs when restricted blood flow to the heart muscle does not cause pain, leading to unnoticed and progressive damage to the heart over time.
Think of arteriosclerosis as a traffic jam in your body’s highway system. Healthy arteries are like clear, unobstructed roads that allow blood to flow freely, delivering oxygen and nutrients to vital organs. However, when arteriosclerosis creates blockages, it is akin to a traffic jam, preventing the smooth passage of blood. As a result, essential organs are deprived of oxygen and nutrients, leading to their malfunction.
Understanding these complications emphasizes the importance of early detection and management of arteriosclerosis to prevent severe health outcomes.
Management and Prevention
Managing arteriosclerosis requires a multifaceted approach that includes both lifestyle changes and, in some cases, medical treatments. To easily remember the key aspects of managing arteriosclerosis, consider the mnemonic ‘HEALTH’: Healthy diet, Exercise, Avoid smoking, Lower cholesterol, Treat hypertension, and Healthy weight.
First and foremost, a healthy diet is crucial. This involves consuming a balanced diet rich in fruits, vegetables, whole grains, and lean proteins while minimizing the intake of saturated fats, trans fats, and processed sugars. Such dietary practices help in maintaining optimal cholesterol levels and reducing the build-up of plaque in the arteries.
Regular exercise plays an essential role in managing arteriosclerosis. Engaging in physical activities such as walking, swimming, or cycling for at least 30 minutes most days of the week helps in improving cardiovascular health, enhancing blood circulation, and maintaining a healthy weight.
Another critical factor is to avoid smoking. Smoking accelerates the hardening of arteries and significantly increases the risk of arteriosclerosis. Quitting smoking can dramatically improve cardiovascular health and reduce the risk of heart attacks and strokes.
Additionally, it’s important to lower cholesterol levels. High cholesterol can lead to plaque formation in the arteries, so consuming cholesterol-lowering foods and, if necessary, taking prescribed medications can help manage this condition effectively.
Treating hypertension is also vital. High blood pressure can damage the arteries over time, leading to arteriosclerosis. Regular monitoring and medications, along with lifestyle changes, can keep blood pressure levels in check.
Maintaining a healthy weight is the final piece of the puzzle. Excess weight can contribute to hypertension and high cholesterol, thus increasing the risk of arteriosclerosis. A balanced diet and regular exercise are key to achieving and sustaining a healthy weight.
In some cases, medications such as statins to lower cholesterol, antihypertensive drugs, or antiplatelet agents may be required. For more severe cases, surgical interventions like angioplasty or coronary artery bypass grafting (CABG) might be necessary. Think of managing arteriosclerosis like giving your car regular maintenance—keeping everything in good working order to ensure smooth operation and longevity.