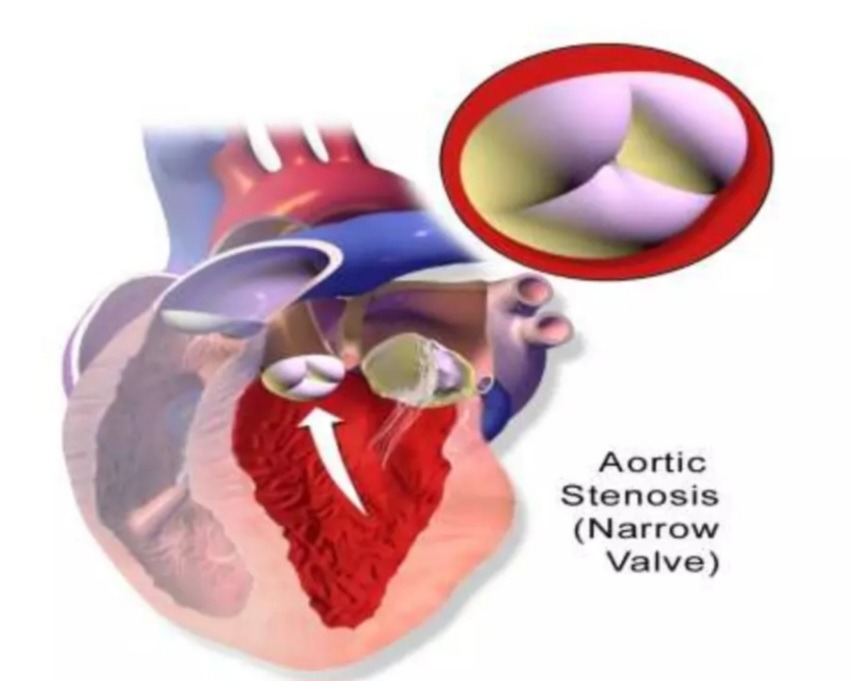
What is Aortic Stenosis?
Aortic stenosis is a medical condition characterized by the narrowing of the aortic valve in the heart. To visualize this, imagine trying to push a significant amount of water through a very narrow straw. The effort required to get the water through is substantially greater than if the straw were wider. Similarly, in aortic stenosis, the heart must exert extra effort to pump blood through the constricted aortic valve.
The mnemonic ‘Stenosis = Straw Narrowing’ can be helpful in recalling this concept. In simpler terms, think of the aortic valve as a gate that regulates the flow of blood from the heart to the rest of the body. When someone has aortic stenosis, this gate becomes partially stuck and does not open fully. As a result, the heart needs to work harder to push blood through this narrow opening, which can lead to a variety of complications.
This condition can develop due to several factors, including aging, congenital heart defects, or the buildup of calcium deposits on the valve. The narrowing restricts the valve’s ability to open fully, thereby impeding efficient blood flow and increasing the workload on the heart. Over time, this increased workload can cause the heart muscle to thicken and weaken, potentially leading to heart failure if left untreated.
Understanding the mechanics of aortic stenosis is crucial for grasping its implications on overall heart function. The heart’s increased effort to pump blood through the narrowed valve can lead to symptoms such as chest pain, shortness of breath, and fatigue. In severe cases, it may result in fainting or even sudden cardiac death. Therefore, early diagnosis and treatment are essential to manage the condition effectively.
Signs and Symptoms
Imagine feeling exhausted and short of breath after a brief walk. This scenario is not uncommon for individuals suffering from aortic stenosis. The condition presents itself through a variety of signs and symptoms that can range from mild to severe over time. To help remember the most common symptoms, you can use the mnemonic “3 Cs”: Chest pain, Collapse (fainting), and Can’t breathe (shortness of breath).
Chest pain or angina is often one of the first indicators of aortic stenosis. This pain typically occurs during physical activity when the heart works harder to pump blood through the narrowed aortic valve. It feels similar to the discomfort experienced during a heart attack. The next significant symptom is collapse or fainting spells, medically referred to as syncope. These episodes can happen suddenly and are usually triggered by physical exertion or emotional stress.
Shortness of breath, or the sensation that you “can’t breathe,” is another hallmark symptom. This occurs because the heart struggles to pump enough blood to meet the body’s needs, leading to fluid build-up in the lungs and causing difficulty in breathing. This symptom might initially present itself only during physical activity but can progress to occur even at rest as the condition worsens.
It’s important to note that aortic stenosis symptoms often develop gradually. In the early stages, you might not notice anything unusual, or you might attribute the subtle symptoms to aging or lack of fitness. However, as the condition progresses, these symptoms become more pronounced and frequent, significantly impacting your quality of life. Think of it like a car engine that starts to misfire; at first, the problem is barely noticeable, but over time, the engine struggles more and more to run smoothly.
Understanding these signs and symptoms is crucial for early detection and management of aortic stenosis. If you or someone you know experiences these symptoms, it’s essential to seek medical evaluation to prevent further complications.
Causes of Aortic Stenosis
Aortic stenosis, a condition characterized by the narrowing of the aortic valve, can arise from several distinct causes. To better understand these causes, we can use the mnemonic ‘CCR’: Calcium buildup, Congenital heart defects, and Rheumatic fever.
Firstly, calcium buildup is a primary cause of aortic stenosis. Over time, calcium deposits can accumulate on the aortic valve, much like tiny rocks, leading to its stiffening and narrowing. This calcification process is more prevalent in older adults and progressively restricts the valve’s ability to open fully, thereby impeding blood flow from the heart to the rest of the body.
Secondly, congenital heart defects can also lead to aortic stenosis. Some individuals are born with aortic valves that are not properly formed, resembling a gate that never opened correctly. This congenital defect can manifest as a bicuspid aortic valve, where the valve has only two leaflets instead of the usual three. Such structural abnormalities can cause the valve to function inadequately, leading to stenosis from an early age.
Lastly, rheumatic fever, a complication of untreated strep throat, can result in aortic stenosis. This condition can cause inflammation and scarring of the aortic valve, making it thick and inflexible. The scarring restricts the valve’s movement, reducing its efficiency and contributing to stenosis. Rheumatic fever as a cause of aortic stenosis is less common in developed countries due to the widespread use of antibiotics but remains a significant concern in regions with limited access to healthcare.
Understanding these causes—calcium buildup, congenital defects, and rheumatic fever—provides a comprehensive overview of the factors contributing to aortic stenosis. Recognizing these causes can help in early diagnosis and effective management of this condition.
Risk Factors
Aortic stenosis is a condition that can develop due to various risk factors, which can be likened to the wear and tear a machine experiences over time. Understanding these risk factors is crucial for early detection and management. One helpful mnemonic to remember these risk factors is “OARS”: Older age, Arteries (high blood pressure and cholesterol), Rheumatic fever, and Smoking.
First and foremost, older age is a significant risk factor. As we age, the aortic valve is prone to calcification, leading to its narrowing. This process is akin to the gradual buildup of scale within a pipe, which restricts water flow over time.
Next, conditions affecting the arteries, such as high blood pressure and high cholesterol, play a pivotal role. High blood pressure exerts additional stress on the heart, causing the valve to work harder and potentially leading to its narrowing. Similarly, high cholesterol can lead to the deposition of fatty substances on the valve, further contributing to its stenosis.
Another critical factor is a history of rheumatic fever. This inflammatory disease, often resulting from untreated strep throat, can cause damage to the heart valves, including the aortic valve. The scarring and thickening of the valve due to rheumatic fever can significantly increase the risk of aortic stenosis later in life.
Finally, smoking is a well-known risk factor for numerous cardiovascular diseases, including aortic stenosis. The harmful substances in tobacco smoke can damage the blood vessels and the heart, exacerbating the likelihood of valve narrowing.
By recognizing these risk factors—Older age, Arteries (high blood pressure and cholesterol), Rheumatic fever, and Smoking—we can better understand who might be at increased risk for developing aortic stenosis. Early identification and proactive management of these factors can play a vital role in mitigating the progression of this condition.
Complications
Aortic stenosis, if left untreated, can lead to severe and life-threatening complications. To understand the gravity of these complications, think of the condition as a dam that might burst if pressure builds up excessively. The mnemonic ‘HSS’ is useful to remember the potential consequences: Heart failure, Stroke, and Sudden death.
Heart failure is one of the most common complications of untreated aortic stenosis. As the aortic valve narrows, the heart must work harder to pump blood through the constricted opening. Over time, this increased workload can weaken the heart muscles, leading to heart failure. Symptoms of heart failure include shortness of breath, fatigue, swelling in the legs and ankles, and persistent coughing or wheezing.
Another critical complication is a stroke. The narrowed aortic valve can cause turbulent blood flow, which may lead to the formation of blood clots. If a blood clot travels to the brain, it can lead to a stroke, depriving brain tissue of essential oxygen and nutrients. The result can be devastating, causing long-term disability or even death. Symptoms of a stroke include sudden numbness or weakness, especially on one side of the body, confusion, difficulty speaking, and loss of coordination or balance.
Perhaps the most alarming complication is sudden death. This can occur without warning, as the heart may suddenly be unable to cope with the increased pressure. Sudden death is often due to an irregular heartbeat or severe heart failure. It underscores the critical importance of early diagnosis and treatment of aortic stenosis.
In summary, the complications of untreated aortic stenosis can be severe and life-threatening. Heart failure, stroke, and sudden death are the primary risks, each with its own set of serious consequences. Recognizing the symptoms and seeking timely medical intervention is crucial to prevent these potentially fatal outcomes.
Management and Treatment
Managing aortic stenosis often involves a combination of medications, lifestyle changes, and surgical interventions. This approach can be easily remembered through the mnemonic ‘MLS’: Medications, Lifestyle, and Surgery.
Medications are typically the first line of defense. They do not cure aortic stenosis but can help relieve symptoms and improve quality of life. Common medications include diuretics, which help reduce fluid buildup, beta-blockers, which lower blood pressure, and statins, which manage cholesterol levels. These medications can be likened to oiling a rusty gate, providing temporary relief and smoother functioning.
Lifestyle changes play a crucial role in managing aortic stenosis. A heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins is essential. Regular physical activity, such as walking or swimming, can strengthen the heart and improve overall cardiovascular health. Quitting smoking and limiting alcohol intake are also recommended. These changes are akin to maintaining the gate regularly to prevent further damage.
When medications and lifestyle changes are insufficient, surgical interventions may be necessary. The most common surgical treatment for aortic stenosis is aortic valve replacement (AVR). This procedure involves replacing the damaged valve with a mechanical or biological valve. Another less invasive option is transcatheter aortic valve replacement (TAVR), which is performed through a catheter inserted into a blood vessel. These surgeries are comparable to replacing a broken gate entirely, ensuring it functions properly again.
In summary, managing aortic stenosis effectively requires a comprehensive approach involving medications, lifestyle modifications, and, when necessary, surgical interventions. By understanding and implementing these strategies, individuals can significantly improve their quality of life and mitigate the symptoms associated with this condition.