What is Tricuspid Valve Regurgitation?
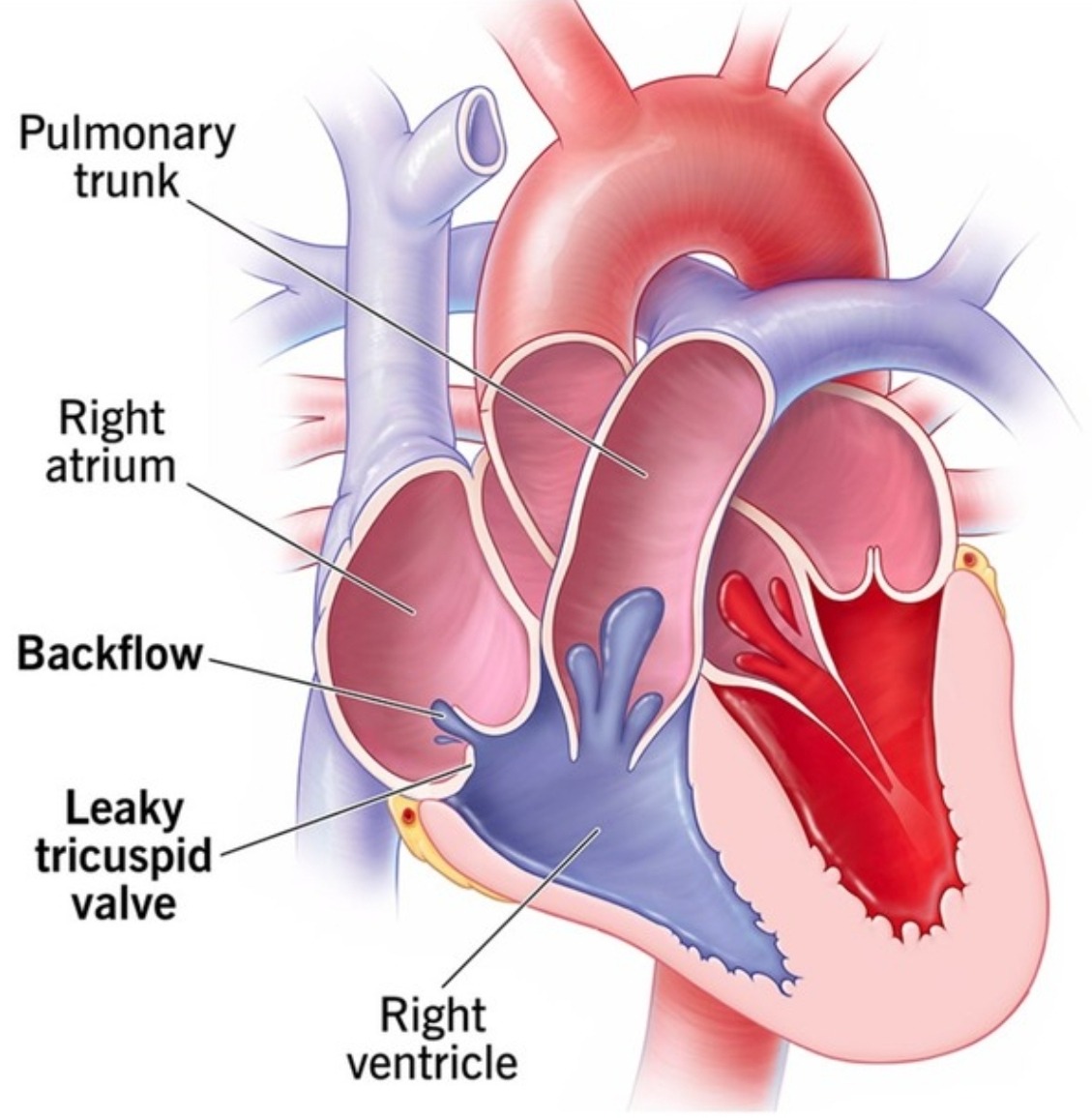
The human heart is a complex organ with four chambers: two upper chambers called atria and two lower chambers called ventricles. The tricuspid valve is located between the right atrium and the right ventricle. It functions much like a door, allowing blood to flow from the right atrium to the right ventricle, and then closing tightly to prevent any backflow of blood.
In a healthy heart, the tricuspid valve ensures that blood flows in one direction and does not leak back into the right atrium. However, in the case of tricuspid valve regurgitation, this valve does not close properly. Imagine a pump that has a faulty valve; instead of water being pushed out efficiently, some of it leaks back into the pump. Similarly, when the tricuspid valve is inefficient, blood leaks back into the right atrium instead of moving forward to the lungs for oxygenation.
This backflow can cause the right atrium to enlarge and eventually lead to increased pressure in the right side of the heart. Over time, this added strain can cause complications such as arrhythmias, heart failure, or other cardiovascular issues. The severity of tricuspid valve regurgitation can vary from mild to severe, and it may be discovered incidentally or through symptoms like fatigue, swelling of the legs, or shortness of breath.
By visualizing the heart as a pump and the tricuspid valve as a door that should close tightly, it becomes easier to understand the implications of regurgitation. A faulty door in a pump system leads to inefficiency and potential damage, just as a malfunctioning tricuspid valve can disrupt the normal flow of blood and strain the heart. Understanding this basic anatomy and function is essential for comprehending the complexities of tricuspid valve regurgitation and its impact on overall health.
Symptoms and Signs: How to Spot Tricuspid Valve Regurgitation
Tricuspid valve regurgitation (TVR) can present a variety of symptoms, some of which may develop gradually and be easily overlooked. Recognizing these symptoms early is crucial for timely medical intervention. One helpful mnemonic for remembering the key symptoms of TVR is ‘FATTY’: Fatigue, Abdominal swelling, Tiredness, Trouble breathing, and Yellow skin.
Fatigue: One of the most common indicators of TVR is persistent fatigue. Individuals may find themselves feeling unusually tired even after light activities such as walking short distances or performing daily chores. This fatigue occurs because the heart is not pumping blood efficiently, leading to decreased oxygen delivery to the body.
Abdominal Swelling: Another telltale sign is swelling in the abdomen, medically known as ascites. This occurs due to fluid accumulation resulting from poor blood circulation. Patients might notice their clothes fitting tighter around the waist or experience discomfort and bloating.
Tiredness: Beyond general fatigue, individuals with TVR often report a profound sense of tiredness. This goes beyond normal tiredness and can severely impact daily activities and overall quality of life. The heart’s inability to pump effectively means that the body is constantly working harder to maintain normal function.
Trouble Breathing: Difficulty breathing or shortness of breath, especially during physical activity or when lying flat, can also be a sign of TVR. This symptom arises because fluid can back up into the lungs, making it difficult to breathe. Patients may find themselves waking up at night feeling short of breath or needing to use multiple pillows to sleep comfortably.
Yellow Skin: In some cases, TVR may lead to a yellowish tint in the skin or eyes, known as jaundice. This can occur when liver function is affected due to prolonged congestion in the hepatic veins.
Practical examples of these symptoms include feeling excessively tired after climbing a flight of stairs, noticing swelling in the feet and ankles by the end of the day, or experiencing shortness of breath while lying down. Recognizing these signs early can lead to more effective management and better outcomes for those with tricuspid valve regurgitation.
Causes: Why Does Tricuspid Valve Regurgitation Happen?
Tricuspid valve regurgitation can arise from various sources, each contributing to the condition in its unique way. Understanding these causes is essential, as it can help in both prevention and management of the disease.
Congenital from birth, or infection’s stealth,
Heart’s own wear and tear, can lead to this affair.These poetic lines encapsulate the primary causes of tricuspid valve regurgitation.
In some cases, individuals are born with congenital defects that impact the tricuspid valve. These defects can cause the valve to malfunction, leading to improper blood flow from the right atrium to the right ventricle.
Another common cause is rheumatic fever, an inflammatory disease that can develop after a streptococcal infection, such as strep throat. The inflammation can damage the tricuspid valve, causing it to become scarred and stiff, which in turn leads to regurgitation. For instance, a person who had rheumatic fever during childhood might develop tricuspid valve regurgitation later in life due to the lingering effects of the disease.
Heart conditions such as right ventricular dilation or failure can also contribute to tricuspid valve regurgitation. When the right ventricle enlarges, it can pull the tricuspid valve apart, preventing it from closing properly. This often occurs in conditions like pulmonary hypertension, where increased blood pressure in the lungs puts added strain on the right side of the heart.
Infections like infective endocarditis, which involves the inner lining of the heart, can also lead to tricuspid valve regurgitation. Bacteria or other pathogens can infect the tricuspid valve, causing it to become damaged and leaky.
In essence, tricuspid valve regurgitation can result from a variety of factors, including congenital defects, infections, and heart conditions. Recognizing these causes can aid in early diagnosis and effective treatment, ultimately improving patient outcomes.
Diagnosis: How Do Doctors Find Out?
Diagnosing tricuspid valve regurgitation involves a series of steps that doctors take to confirm the condition and understand its severity. These steps usually begin with a physical examination, where the doctor listens to the heart using a stethoscope. Abnormal heart sounds, like a murmur, might indicate a problem with the tricuspid valve. However, to get a clearer picture, doctors rely on more advanced diagnostic tools.
One of the primary methods used is an echocardiogram. This test is similar to taking a video of the heart in action. It uses sound waves to create detailed images of the heart’s structure and function. Through an echocardiogram, doctors can observe how well the tricuspid valve is working and determine if there is any regurgitation, which is the backward flow of blood through the valve.
To complement the echocardiogram, doctors might also order a chest X-ray. This imaging test provides a visual of the heart and lungs, helping to identify any enlargement of the heart or fluid buildup in the lungs, which can be indicative of tricuspid valve regurgitation. Together, these tests offer a comprehensive view of the heart’s condition.
Let’s consider a real-life scenario. Imagine a patient named Sarah, who has been experiencing fatigue and shortness of breath. Concerned, she visits her doctor, who performs a physical exam and hears a murmur. Suspecting a heart valve issue, the doctor orders an echocardiogram. The results reveal that Sarah’s tricuspid valve is not closing properly, causing regurgitation. To further assess the impact on her heart and lungs, a chest X-ray is conducted, confirming the diagnosis.
Through these diagnostic steps, doctors can accurately identify tricuspid valve regurgitation and develop an appropriate treatment plan tailored to the patient’s needs. This systematic approach ensures that conditions affecting heart valves are effectively managed, improving patient outcomes.
Treatment Options: What Can Be Done?
When addressing tricuspid valve regurgitation, a range of treatment options are available, from conservative lifestyle changes to more invasive surgical procedures. To help remember these options, consider the mnemonic ‘MEDS’ – Medications, Exercise, Diet, Surgery.
Medications: The first line of treatment often involves medications aimed at managing symptoms and preventing complications. Diuretics are commonly prescribed to reduce fluid buildup, thereby alleviating swelling and discomfort. In some cases, patients might also be given medications to manage underlying conditions such as atrial fibrillation or high blood pressure, which can exacerbate tricuspid valve regurgitation.
Exercise: Regular physical activity can be beneficial, but it must be tailored to the individual’s condition. A healthcare provider may recommend a specific exercise regimen that avoids excessive strain on the heart. For instance, moderate aerobic activities like walking or swimming can improve cardiovascular health without overburdening the tricuspid valve.
Diet: Dietary changes are another cornerstone of managing tricuspid valve regurgitation. Patients are often advised to reduce their salt intake to prevent fluid retention, which can worsen symptoms. Incorporating heart-healthy foods, such as fruits, vegetables, and whole grains, can also support overall cardiovascular health. For example, a patient might be encouraged to swap out processed foods for fresh, nutrient-dense options to help manage their condition more effectively.
Surgery: In more severe cases, surgical intervention may be necessary. Options include valve repair or valve replacement surgeries. Valve repair might involve procedures to reshape or tighten the valve, while valve replacement entails installing a new prosthetic valve. For example, a patient with significant symptoms and deteriorating heart function might undergo valve repair surgery to restore normal valve function and improve quality of life.
Each treatment pathway is tailored to the individual’s specific needs, and a comprehensive approach often involves a combination of these strategies. Consulting with a healthcare provider is crucial to determine the most appropriate plan based on the severity of the condition and the patient’s overall health.
Living with Tricuspid Valve Regurgitation: Tips for Everyday Life
Living with tricuspid valve regurgitation requires a balanced approach to daily habits. Think of your heart as a garden; it needs regular care and attention to bloom. A heart-healthy diet is crucial. Focus on consuming plenty of fruits, vegetables, whole grains, and lean proteins while minimizing salt and saturated fats. These dietary choices help maintain optimal heart function and overall well-being.
Regular exercise is another key component. Aim for moderate activities like walking, swimming, or cycling, which can boost cardiovascular health without overburdening your heart. However, it’s essential to consult with your healthcare provider before starting any new exercise regimen to ensure it aligns with your condition and capabilities.
Tracking symptoms in a journal can be immensely beneficial. Record any changes in your condition, such as fatigue, shortness of breath, or swelling in your legs. This practice provides valuable insights for your medical team, allowing them to adjust treatment plans effectively. Additionally, it helps you become more attuned to your body’s signals, facilitating prompt medical consultations if needed.
Regular medical check-ups are indispensable for managing tricuspid valve regurgitation. These appointments enable your healthcare provider to monitor your condition closely, adjust medications, and recommend tests or procedures as necessary. Staying informed about your condition and treatment options empowers you to make educated decisions about your health.
Lastly, maintaining open communication with your healthcare team cannot be overstated. Feel free to ask questions, express concerns, and seek clarification when needed. Your proactive involvement in your care plan can significantly improve your quality of life, ensuring that your heart continues to function as efficiently as possible.