Introduction to Pulmonary Regurgitation
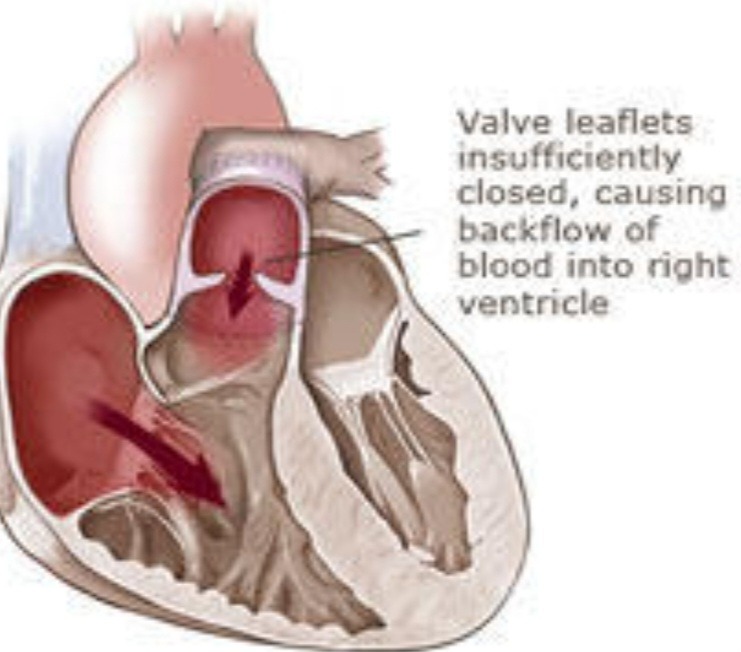
Pulmonary regurgitation (PR) is a condition characterized by the improper closure of the pulmonary valve, allowing blood to flow backward into the right ventricle from the pulmonary artery. To put it simply, think of the pulmonary valve as a door that should close tightly to keep blood flowing in one direction. When this door doesn’t close properly, it permits blood to leak back into the heart, much like a door that doesn’t shut all the way allows air to seep back into a room. This backward blood flow is known as regurgitation.
The significance of understanding pulmonary regurgitation lies in its impact on heart function and overall health. The heart’s primary role is to pump oxygen-rich blood throughout the body, ensuring that all organs and tissues receive the oxygen and nutrients they need. When the pulmonary valve malfunctions, it disrupts the efficient flow of blood, potentially leading to various complications over time. For instance, the right ventricle may become enlarged or weakened from having to work harder to compensate for the backward flow, eventually affecting the entire cardiovascular system.
While PR might sound alarming, it’s important to note that not all cases are severe. The severity of the condition can vary widely, from mild cases that require little to no treatment to more severe situations that necessitate medical intervention. Early detection and a comprehensive understanding of pulmonary regurgitation are crucial in managing the condition effectively and maintaining heart health.
In the following sections, we will delve deeper into the causes, symptoms, diagnosis, and treatment options for pulmonary regurgitation. By breaking down each aspect, we aim to provide a comprehensive yet accessible resource for anyone seeking to understand this heart condition. Whether you’re a patient, a caregiver, or simply someone interested in learning more about heart health, this guide will offer valuable insights into pulmonary regurgitation and its implications.
How The Heart Works: A Quick Refresher
To comprehend pulmonary regurgitation, it is essential first to understand the normal functioning of the heart. The human heart is a muscular organ divided into four chambers: two atria on the top and two ventricles at the bottom. Blood flows through these chambers, regulated by four critical valves: the tricuspid valve, the pulmonary valve, the mitral valve, and the aortic valve.
The heart operates like a well-coordinated pump, where the right side (right atrium and right ventricle) handles deoxygenated blood, while the left side (left atrium and left ventricle) deals with oxygenated blood. To make it easier to remember, use the mnemonic ‘LORD’: ‘Left, Oxygenated, Right, Deoxygenated.’
Here’s a short rhyme to help you recall:
Left is for life, with oxygen anew,
Right is for rest, where old blood flows through.
Chambers and valves work hand in hand,
To keep you healthy, across our land.
In this system, the pulmonary valve plays a pivotal role. Positioned between the right ventricle and the pulmonary artery, it ensures that blood flows from the heart to the lungs without backflow. When the right ventricle contracts, the pulmonary valve opens to allow deoxygenated blood to travel to the lungs for oxygenation. Upon relaxation, the valve closes to prevent the blood from flowing back into the heart.
Understanding the normal operation of the heart, especially the pulmonary valve, sets the stage for grasping the implications when this process is disrupted, as in pulmonary regurgitation. This condition occurs when the pulmonary valve does not close entirely, leading to the backward flow of blood into the right ventricle.
What Causes Pulmonary Regurgitation?
Pulmonary regurgitation (PR) arises from multiple etiologies, ranging from congenital heart defects to acquired conditions. Understanding the specific causes can help demystify this complex cardiac issue. One primary cause of PR is congenital heart defects, which are present at birth. These defects can involve structural abnormalities in the heart’s valves or chambers, leading to improper valve function and, consequently, pulmonary regurgitation.
Another significant cause is infectious diseases, such as infective endocarditis. This condition involves an infection of the heart’s inner lining, often affecting the pulmonary valve and impairing its function. The resultant damage can lead to the valve’s inability to close properly, causing PR. Additionally, rheumatic fever, a complication of untreated strep throat, can cause similar damage to the heart valves, including the pulmonary valve.
Heart conditions acquired later in life, such as pulmonary hypertension or chronic pulmonary embolism, can also lead to PR. These conditions impose excessive pressure on the pulmonary valve, eventually leading to its malfunction. It is noteworthy that surgical interventions for other heart issues, such as valve replacement or repair, may inadvertently affect the pulmonary valve, leading to regurgitation.
To illustrate, consider the story of a young athlete who was diagnosed with PR during a routine check-up. Initially, the athlete experienced mild symptoms like shortness of breath during intense training sessions. Further examination revealed that he was born with a minor heart defect that went unnoticed for years. Over time, this congenital abnormality led to the development of pulmonary regurgitation. This scenario demonstrates how PR can originate from congenital issues and remain undetected until later in life. Understanding these causes helps in early identification and management of the condition, ensuring better outcomes for those affected.
Symptoms and Diagnosis of Pulmonary Regurgitation
Pulmonary regurgitation (PR) manifests through a variety of symptoms that can affect day-to-day life. One of the most common signs is shortness of breath, which can feel as though you’re trying to breathe through a straw. This difficulty in breathing often intensifies during physical activity or when lying flat. Another prevalent symptom is fatigue; individuals with PR may find themselves feeling unusually tired, even after minimal exertion or adequate rest.
Heart murmurs are another key indicator of PR. A heart murmur is an unusual sound heard between heartbeats, often described as a whooshing or swishing noise. This occurs due to turbulent blood flow and can be detected by a healthcare provider using a stethoscope. Irregular heartbeats, also known as arrhythmias, are yet another symptom. These irregularities can feel like fluttering or pounding in the chest and may cause dizziness or fainting spells.
To aid in remembering these symptoms, the mnemonic ‘FISH’ can be useful: ‘Fatigue, Irregular Heartbeats, Shortness of Breath, Heart Murmurs.’
Diagnosing pulmonary regurgitation involves a combination of clinical evaluation and diagnostic tests. Initially, a doctor will listen to the heart using a stethoscope to detect any abnormal sounds such as murmurs. This preliminary examination can provide valuable clues about the condition of the heart and the presence of PR.
Further diagnostic confirmation is typically achieved through an echocardiogram, a specialized ultrasound of the heart. This test allows doctors to visualize the heart’s structure and function, including the movement of blood through the pulmonary valve. An echocardiogram can provide detailed images that help assess the severity of the regurgitation.
Additional tests may include a chest X-ray, which can show changes in the size and shape of the heart, and an electrocardiogram (ECG) to evaluate the heart’s electrical activity. In some cases, more advanced imaging techniques like cardiac MRI or CT scans may be employed to gain a comprehensive understanding of the heart’s condition and confirm the diagnosis of pulmonary regurgitation.
Treatment Options and Management
Pulmonary regurgitation (PR) is a condition that, while serious, can be effectively managed with a range of treatment options. These treatments can be broadly categorized into lifestyle changes, medications, and surgical interventions. Understanding these options can empower individuals with PR to take proactive steps towards better health.
First and foremost, lifestyle changes are often recommended to help manage PR. This might include adjustments to one’s diet and exercise routine. For example, a person with PR may be advised to limit their intake of sodium, which can help reduce fluid retention and alleviate the strain on the heart. Regular, moderate exercise can also be beneficial, although it is crucial to consult with a healthcare provider to determine the most appropriate level of physical activity.
Medications are another cornerstone of PR management. Diuretics, for instance, help remove excess fluid from the body, easing the burden on the heart. Beta-blockers may be prescribed to help control heart rate and lower blood pressure, which can improve heart function. It is essential for patients to adhere to their prescribed medication regimen and have regular follow-ups with their healthcare provider to monitor their condition.
In more severe cases, surgical interventions may be necessary. One common procedure is pulmonary valve replacement, where the damaged valve is replaced with a prosthetic one. This surgery can significantly improve symptoms and quality of life for individuals with advanced PR. Less invasive procedures, such as balloon valvuloplasty, may also be considered depending on the specifics of the case.
To illustrate the effectiveness of these treatments, consider the story of Jane, a 45-year-old woman diagnosed with PR. After experiencing fatigue and shortness of breath, Jane consulted her cardiologist. She was advised to make dietary changes, incorporate light exercise, and take prescribed medications. Over time, Jane’s symptoms improved significantly, and she was able to resume her daily activities without major interruptions. Her inspiring journey underscores the importance of a comprehensive and tailored approach to managing PR.
Overall, while pulmonary regurgitation can be daunting, a combination of lifestyle changes, medications, and surgical options provides a robust framework for effective management. With proper care and guidance, individuals with PR can lead fulfilling and healthy lives.
Living with Pulmonary Regurgitation: Tips and Advice
Living with pulmonary regurgitation (PR) can pose unique challenges, but with the right strategies and lifestyle adjustments, individuals can effectively manage their condition and lead fulfilling lives. Here are some practical tips to help monitor symptoms, stay active, and maintain a heart-healthy lifestyle.
Monitoring Symptoms: Regularly tracking symptoms is crucial for effective management of PR. Keep a journal to note any changes in how you feel, including shortness of breath, fatigue, or swelling in the legs and feet. Use a consistent format to record your entries, which can make it easier to identify patterns over time. It’s important to attend all scheduled medical appointments and communicate any new or worsening symptoms to your healthcare provider promptly.
Staying Active: Physical activity is beneficial for overall cardiovascular health, but it’s essential to choose exercises that are safe and appropriate for your condition. Low-impact activities such as walking, swimming, and cycling are generally recommended. Consult with your doctor or a physical therapist to create a personalized exercise plan that aligns with your capabilities and limitations. Remember to listen to your body and take breaks when necessary.
Maintaining a Heart-Healthy Lifestyle: A heart-healthy diet plays a significant role in managing pulmonary regurgitation. Focus on incorporating plenty of fruits, vegetables, whole grains, lean proteins, and healthy fats into your meals. Limit your intake of salt, sugar, and saturated fats to help control blood pressure and reduce strain on your heart. Additionally, avoid smoking and limit alcohol consumption, as these habits can exacerbate heart conditions.
To make these tips easy to remember, consider this simple rhyme:
“Monitor, move, and eat with care,
These are the ways to stay aware.
Track your symptoms day by day,
Stay active in a heart-safe way.
Healthy food on your plate,
Keeps your heart in good state.”
By following these practical tips, individuals with pulmonary regurgitation can take proactive steps to manage their condition and enhance their quality of life.