Introduction to Pericarditis
Pericarditis is a medical condition characterized by the inflammation of the pericardium, the protective sac that surrounds the heart. To visualize this, imagine the pericardium as a plastic bag safeguarding a piece of fruit. When this protective bag becomes inflamed, it can lead to discomfort and a range of other symptoms. A memorable way to understand this is through a rhyme: ‘When the heart’s shield swells, discomfort tells.’ This encapsulates the essence of pericarditis in a simple yet effective manner.
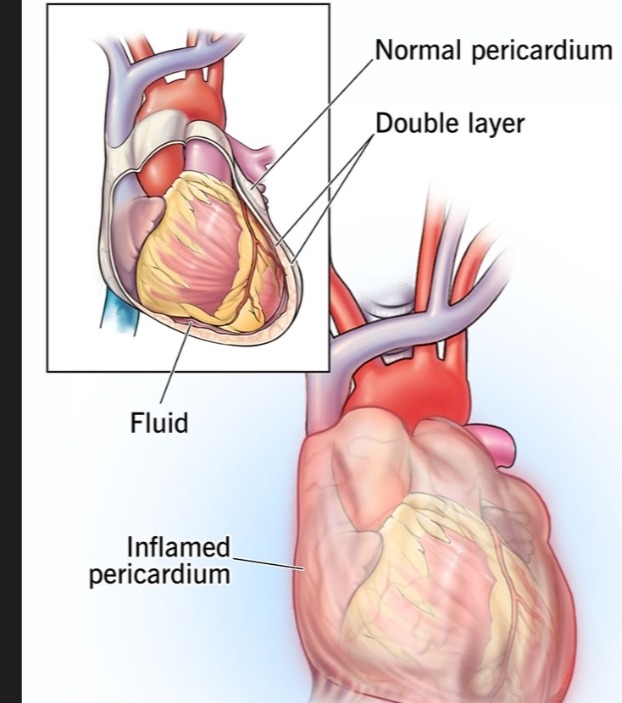
The pericardium consists of two layers: an outer fibrous layer and an inner serous layer. Between these layers is a small amount of fluid that allows them to move smoothly against each other as the heart beats. When inflammation occurs, this fluid can increase, causing the pericardial layers to rub against the heart, leading to chest pain and other symptoms.
The discomfort or pain associated with pericarditis can be sharp or stabbing and is typically felt in the center or left side of the chest. The pain may also travel to the shoulder or neck. Other common symptoms can include a low-grade fever, fatigue, and palpitations. It’s essential to understand that the severity of these symptoms can vary from mild to severe, influencing the patient’s quality of life.
Understanding pericarditis is crucial for recognizing the signs early and seeking prompt medical attention. Early diagnosis can significantly improve the management and treatment of this condition, fostering better patient outcomes. As we delve deeper into the intricacies of pericarditis in the subsequent sections, it will become clear how complex yet manageable this condition can be with appropriate knowledge and care.
Causes of Pericarditis
Pericarditis, an inflammation of the pericardium, can have several underlying causes, which can be tricky to remember. A helpful mnemonic to simplify this is “I V.I.R. C.R.A.C.K.,” which stands for Infections, Virus, Inflammation, Rheumatic conditions, Cancer, Radiation, Auto-immune disorders, Chronic kidney disease, and Kidney failure. Each letter in this mnemonic highlights a significant cause of pericarditis.
First, infections are a frequent cause of pericarditis. This includes bacterial and viral infections. For example, a bacterial infection like tuberculosis or a viral infection such as influenza can lead to this condition. These pathogens can directly infect the pericardium or trigger an inflammatory response.
Second, inflammation plays a critical role. This inflammation could result from direct injury, such as a car accident causing trauma to the chest. When the pericardium becomes inflamed, fluid may accumulate, leading to symptoms associated with pericarditis.
Third, certain rheumatic conditions can lead to pericarditis. For instance, diseases like rheumatoid arthritis or systemic lupus erythematosus, which are autoimmune in nature, cause the body’s immune system to attack its own tissues, including the pericardium.
Fourth, cancer and its treatments can contribute to this condition. Tumors may spread to the pericardium, or radiation therapy (particularly for cancers near the chest) can cause damage and subsequent inflammation.
Lastly, chronic kidney disease and kidney failure are noteworthy contributors. These conditions can lead to uremic pericarditis, where the build-up of waste products in the blood causes inflammation of the pericardium.
Understanding the various causes of pericarditis, from infections to chronic illnesses, can help in recognizing and managing this condition effectively. Remembering the mnemonic “I V.I.R. C.R.A.C.K.” can simplify this complex topic, making it more approachable and easier to recall.
Symptoms of Pericarditis
John, a 45-year-old office worker, started his Monday like any other. As he sipped his morning coffee, an unexpected and sharp chest pain hit him, taking his breath away momentarily. He shrugged it off as a mere muscle strain from a rough night’s sleep and proceeded with his routine. By lunchtime, however, the pain had grown more severe, making it difficult for him to focus on his tasks.
As the day progressed, John noticed the pain was worse when lying down and slightly relieved when he sat up, as though it ebbed and flowed with his posture—a pain that grows when lying low. His discomfort escalated, leading to periods of breathlessness, where taking a full, deep breath felt almost impossible. Along with the chest pain, a nagging fever started to build, adding a layer of fatigue that made every step feel like a marathon.
By the evening, the situation had become unbearable. The pain, now sharp and stabbing, seemed to pulsate with each heartbeat. His wife, alarmed by his distress, urged him to visit the emergency room. Once there, John described his symptoms to the physician. He mentioned the worsening pain when he lay down, a sensation that slightly subsided when he sat up—key indicators of pericarditis. The doctor also noted John’s fever and shortness of breath, classic signs of this inflammation.
John’s story is a common narrative among those suffering from pericarditis. The hallmark symptom is acute chest pain that can be debilitating, varying with body posture. Often, sufferers find little solace until their condition is properly managed. Fever, difficulty breathing, and fatigue accompanying the chest pain are not mere inconveniences but significant symptoms that signal the urgency for medical intervention.
Diagnosis of Pericarditis
The diagnosis of pericarditis involves a systematic approach that combines a thorough evaluation of a patient’s medical history, physical examination, and various diagnostic tests. This can be likened to the methodical process a mechanic would undertake when inspecting a car for issues. An effective mnemonic to remember these steps is ‘HEART TEST’ – History, Examination, ACT (ECG, Echo, and Tests for inflammation).
Firstly, the doctor will discuss the patient’s History. This involves gathering information about any recent infections, surgeries, or underlying health conditions. Just as a mechanic queries the car owner about recent performance issues or past repairs, the medical history illuminates potential triggers or risk factors for pericarditis.
Secondly, a detailed Examination is conducted. This physical examination often focuses on checking for pericardial friction rubs, an abnormal sound heard through a stethoscope indicative of pericarditis. This step mirrors the mechanic’s visual and auditory inspections of the car for obvious signs of malfunction, such as unusual noises or visible wear.
The next steps, encapsulated by ACT, involve diagnostic Tests. An Electrocardiogram (ECG) is typically employed first, as it assesses the heart’s electrical activity and can reveal characteristic changes associated with pericarditis. The mechanic’s equivalent would be running computerized diagnostics to pinpoint electrical faults in the car.
Subsequently, an Echocardiogram (Echo) is often performed. This ultrasound test provides images of the heart, showing any fluid accumulation around the pericardium. Think of this like the mechanic using an endoscope to see within the car engine’s internal parts without disassembly.
Lastly, Tests for inflammation such as blood tests measure markers like CRP and ESR, indicating an inflammatory response in the body. This is akin to the mechanic performing fluid analyses to detect possible contaminants or imbalance, providing a clearer picture of the car’s condition.
In summary, diagnosing pericarditis is a comprehensive process blending clinical expertise and advanced diagnostic tools, ensuring the accurate identification and subsequent management of this complex condition.
“`html
Treatment and Management
Treating and managing pericarditis is a multifaceted approach that requires a thorough understanding of the condition and its underpinnings. The primary goal is to alleviate symptoms and address the root cause when it is identifiable. As the saying goes, ‘Medicate to alleviate, manage to eliminate.’ This sets the stage for an overarching strategy that blends medicinal intervention with daily management practices.
One of the primary treatment methods for pericarditis involves the use of anti-inflammatory medications, such as ibuprofen. These medications help to reduce inflammation and relieve pain, often providing significant symptom relief. For cases where the cause of pericarditis is known, specific treatments are tailored accordingly. For instance, if a bacterial infection is identified, antibiotics are prescribed, whereas autoimmune causes might necessitate corticosteroids or other immunosuppressive drugs.
Effective management of pericarditis can be likened to the care a gardener provides to a flourishing garden. Just as a garden needs regular watering, weeding, and attention to thrive, managing pericarditis requires consistent care and timely responses to arising issues. This involves regular follow-ups with a healthcare provider to monitor the condition and make necessary adjustments to the treatment plan.
Furthermore, lifestyle changes are pivotal in the management of pericarditis. Patients are often advised to rest adequately, as excessive physical activity can exacerbate symptoms. A well-balanced diet that supports overall cardiovascular health is also recommended. Avoiding strenuous activities, particularly during flare-ups, is crucial to prevent aggravation of the condition.
Through a well-rounded approach that combines medication with effective management strategies and lifestyle modifications, individuals with pericarditis can achieve substantial symptom relief and improved quality of life. Consistency and a proactive stance in treatment and management are key to navigating this complex condition.
“`
Living with Pericarditis: Tips and Support
Living with pericarditis can be challenging, but with a proactive approach and the right support, you can effectively manage this condition. Integrating simple, daily routines can significantly improve your quality of life.
First and foremost, maintaining regular doctor visits is crucial for monitoring your progress and symptoms. Your healthcare provider can offer guidance tailored to your situation, ensuring you receive the most appropriate care.
Support groups can also be an invaluable resource. Connecting with others who are experiencing similar challenges can foster a sense of community and provide emotional support. Many online forums and local support groups are dedicated to helping those with pericarditis. They offer a platform to share experiences, advice, and encouragement, which can be immensely comforting.
Another key component of managing pericarditis is symptom monitoring. Keep a diary of your symptoms, noting any changes or patterns. This information can help your doctor adjust your treatment plan as needed. Remember the simple rhyme: “Rest and test, always do your best.” Ensure you get plenty of rest and listen to your body’s signals to avoid overexertion.
Beyond physical health, mental well-being is equally important. Chronic illness can take a toll on mental health, so it’s vital to seek support when needed. Consider speaking with a mental health professional if you feel overwhelmed. Engaging in relaxing activities such as reading, meditation, or hobbies you enjoy can also contribute to a positive mindset.
If you’re looking for additional resources, organizations like the American Heart Association and the National Institutes of Health provide extensive information on pericarditis, including treatment options and lifestyle tips. Moreover, many educational websites and virtual seminars offer insights into living with cardiac conditions.
Remember, you’re not alone in this journey. By staying proactive, seeking support, and focusing on both your physical and mental health, you can navigate life with pericarditis more smoothly and with greater confidence.