What is Myocarditis?
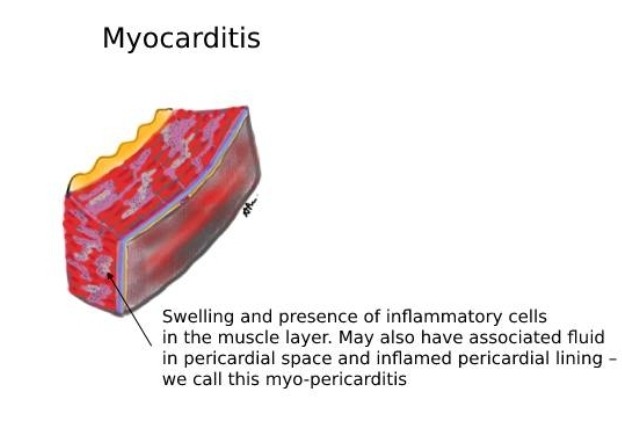
Myocarditis refers to the inflammation of the heart muscle, scientifically known as the myocardium. Imagine your heart as an industrious office worker, constantly bustling to meet the demands of your body. Suddenly, this diligent worker is burdened with unexpected tasks, causing strain and, eventually, disruption in the workflow. This scenario mirrors how myocarditis affects the heart, challenging its ability to function optimally.
This medical condition can touch anyone’s life, irrespective of age, gender, or prior health status. It can strike the most athletic individual as easily as someone with a sedentary lifestyle. The diverse range of people susceptible to myocarditis underscores its unpredictable nature. It’s crucial to understand that myocarditis isn’t selective and can emerge out of nowhere, putting an individual’s cardiac health at risk.
Various factors can instigate myocarditis. Infections, particularly viral ones such as those caused by the Coxsackievirus or SARS-CoV-2, are common triggers. Bacteria, fungi, and other pathogens can also be culpable. Additionally, autoimmune diseases where the body mistakenly attacks its tissues can lead to myocarditis. Examples include lupus and rheumatoid arthritis. Adverse reactions to certain medications or exposure to toxins and chemicals further complicate the list of potential causes.
The broad spectrum of causes demonstrates the complexity behind diagnosing and treating myocarditis. Each case is unique, warranting a comprehensive investigation to identify the specific trigger and tailor the treatment accordingly. Understanding what myocarditis is and recognizing its multifaceted nature is the first step in navigating this stealthy cardiac challenge.
Causes and Risk Factors
Understanding the causes of myocarditis can be pivotal in grasping the comprehensive nature of this heart condition. Using the mnemonic ‘VIRA’ (Viral, Idiopathic, Rheumatic, Autoimmune) helps simplify this complexity for easier recall.
Firstly, viral infections are one of the leading causes of myocarditis. Common viruses, including the influenza virus and the more recent COVID-19 virus, are notorious for triggering this condition. When these viruses invade the body, they can also affect the heart muscle, leading to inflammation. For instance, contracting the flu during its peak season can inadvertently place one at risk for myocarditis, exemplifying a connection between routine activities and health outcomes.
Secondly, the term idiopathic refers to instances where the exact cause of myocarditis remains unknown. Despite thorough medical evaluations, sometimes the origin of the inflammation cannot be pinpointed, which underscores the enigmatic nature of some medical conditions.
Rheumatic fever and related diseases form another cause. Stemming from severe strep throat infections, this illness predominantly affects children and can lead to long-term heart damage if untreated. Engaging in environmental activities that expose individuals to infectious agents, such as crowded environments or shared sports equipment, could heighten the risk.
Lastly, autoimmune disorders represent a significant risk factor. Conditions such as lupus, which cause the immune system to attack its tissues, can inadvertently lead to myocarditis. These chronic illnesses are often accompanied by other health complications, making their management intricate and requiring vigilance towards heart health.
Apart from these primary causes, bacterial infections, environmental toxins, and chronic illnesses also contribute to myocarditis. Exposure to certain bacteria, like those causing Lyme disease, and prolonged contact with harmful chemicals can increase one’s vulnerability. Chronic illnesses, including diabetes and severe allergic reactions, further exacerbate the risk.
Through appreciating the myriad causes and risk factors associated with myocarditis, one can better understand the preventive measures and proactive health strategies essential for protecting heart health.
Symptoms to Watch For
If your heart feels like it’s in a race, with chest pain and a weary face, shortness of breath, and you feel faint, see a doctor, no time to wait!
Myocarditis can present itself through a variety of symptoms, which can sometimes be mistaken for other health issues, making early detection crucial. One of the most common signs of myocarditis is chest pain. This pain may feel sharp or intense, resembling the sensation of a heart attack. It often escalates to the point where it can become unbearable, urging immediate medical attention.
Fatigue is another prominent symptom. This isn’t the kind of tiredness that subsides with a good night’s rest; it’s an overwhelming exhaustion that hinders daily activities. Imagine running errands or climbing stairs only to find yourself unusually worn out or need to rest halfway through tasks that were once routine.
Shortness of breath is also a key indicator of myocarditis. Patients may experience this while performing physical activities or even while at rest. Picture a scenario where a simple walk to the mailbox leaves you gasping for air, a troubling sign that shouldn’t be ignored.
Swelling in the lower extremities, particularly the legs, is another symptom to monitor. This edema is often a result of fluid retention due to the heart’s inability to pump effectively, leading to uncharacteristic puffiness around the ankles and feet.
Dizziness or fainting spells are also warnings not to overlook. The erratic heartbeat and insufficient blood flow to the brain caused by myocarditis can make you feel light-headed or lead to sudden fainting episodes. This may occur without warning and can result in dangerous falls or other injuries.
Real-life scenarios underscore the necessity of recognizing these symptoms early. For example, if someone experiences unusual chest pain and dismisses it as indigestion, they risk severe complications. Similarly, chronic fatigue, when wrongly attributed to a busy lifestyle, might overlook the underlying heart issue. Noticing these symptoms and consulting a healthcare provider can significantly influence outcomes, emphasizing why it’s imperative to stay vigilant about the body’s signals.
Diagnosis: How Doctors Confirm Myocarditis
Diagnosing myocarditis, an inflammation of the heart muscle, involves a comprehensive evaluation by healthcare professionals to confirm its presence and assess its severity. Imagine an MRI as a sophisticated camera that takes detailed images of your heart, allowing doctors to spot inflammation or structural abnormalities. This advanced technique provides a clear picture of the heart’s condition, much like how a high-definition camera captures fine details in a photograph.
Another essential tool in diagnosing myocarditis is the electrocardiogram (ECG), which records the electrical activity of the heart. Think of an ECG as a heart rhythm map revealing any irregularities or abnormalities that might be indicative of inflammation. By analyzing the patterns and rhythms, doctors can detect signs of myocarditis even when symptoms are subtle.
Additionally, blood tests play a crucial role in the diagnostic process. These tests check for markers of inflammation and specific proteins related to heart damage. Elevated levels of certain enzymes or proteins may signal that the heart muscle is under distress. For instance, the presence of troponin, a protein released when the heart is injured, could alert doctors to potential myocarditis.
Consider a practical example to illustrate this process: Emily, a 35-year-old woman, experiences unexplained chest pain and fatigue. Concerned, she consults her doctor, who promptly orders an ECG. The results reveal some irregular rhythms, prompting further investigation with an MRI. The MRI images clearly show areas of inflammation in her heart muscle. Coupled with elevated protein levels found in Emily’s blood tests, her doctor confirms the diagnosis of myocarditis.
The importance of seeking medical attention when experiencing symptoms like chest pain, shortness of breath, or fatigue cannot be overstated. Early diagnosis and intervention are crucial in managing myocarditis effectively, preventing complications, and promoting recovery. Delaying medical evaluation can lead to more severe outcomes, emphasizing the need for timely and comprehensive diagnostic procedures.
Treatment Options
Addressing myocarditis, an often elusive heart condition, necessitates multifaceted treatment strategies. Primarily, medications serve as your heart’s support team, facilitating recovery and minimizing inflammation. Anti-inflammatory drugs, for example, target the root cause by reducing swelling in heart tissues, akin to a support crew managing a critical structure’s repairs. In conjunction, immunosuppressive medications might be prescribed to regulate the immune response, thus preventing further cardiac damage.
In addition to pharmacological interventions, lifestyle modifications play a pivotal role in managing myocarditis. Rest is paramount, akin to handing the reins over to your body’s natural healing processes. Restricting physical activity allows the heart to recover without undue strain. Incorporating a heart-healthy diet, rich in fruits, vegetables, and whole grains, nourishes the body while supporting overall cardiovascular health. Avoiding alcohol and tobacco products also alleviates stress on the heart, fostering an environment conducive to healing.
In more severe instances, advanced interventions may become necessary. For some, the introduction of a pacemaker helps normalize the heart’s rhythm, ensuring it beats in a steady, controlled manner. This device acts like an orchestra conductor, guiding the heart’s rhythm to maintain harmony. In critical situations where the heart’s function is significantly impaired, surgical options, including heart transplants, stand as viable solutions, addressing the root issue at a more fundamental level.
Effective home care and rehabilitation are critical components of the recovery journey. Adhering to medical advice and prescribed medication regimens cannot be overstated. Regular follow-up appointments are vital to monitor progress and adjust treatments as necessary. Incorporating low-impact exercises, once approved by a healthcare provider, helps improve heart function over time. Equally important is fostering a support network comprising family, friends, and healthcare professionals, providing emotional and practical assistance throughout the recovery process.
Prevention and Living with Myocarditis
Adopting proactive measures is paramount in preventing myocarditis and managing life post-diagnosis. To simplify these strategies, let’s consider the mnemonic ‘HEART’: Healthy lifestyle, Early treatment, Avoid risky behaviors, Regular check-ups, and Take medications.
Healthy Lifestyle: Embracing a healthy lifestyle is foundational. This includes a balanced diet rich in fruits, vegetables, lean proteins, and whole grains. Incorporate regular physical activity tailored to your capability and avoid excessive alcohol consumption. Staying hydrated and ensuring sufficient rest are also crucial for overall cardiovascular health.
Early Treatment: Promptly addressing infections and illnesses plays a critical role. If symptoms like chest pain, fatigue, or shortness of breath arise, seek medical attention immediately. Timely intervention can mitigate the progression of myocarditis, lessening its impact.
Avoid Risky Behaviors: Engage in behaviors that minimize your risk of infections. This means maintaining good hygiene practices such as regular handwashing and ensuring vaccinations are updated, particularly against common viruses like influenza and COVID-19. Moreover, avoiding the use of illicit drugs can prevent potential heart damage.
Regular Check-ups: Routine medical check-ups allow for early detection and management of potential health issues. Regular monitoring can identify changes in heart function, facilitating appropriate adjustments to your treatment plan.
Take Medications: Adhering to prescribed medications is essential for those diagnosed with myocarditis. These might include anti-inflammatory drugs, diuretics, or medications to manage heart rhythm and blood pressure. Consistent use as directed by your healthcare provider ensures optimal management of the condition.
Living with myocarditis is a journey that requires adapting and optimizing one’s lifestyle. However, many individuals successfully manage their condition and lead fulfilling lives. For instance, Sarah, a young professional, was diagnosed with myocarditis at 28. Through a combination of medication adherence, regular exercise, and maintaining a balanced diet, she continues to pursue her career and hobbies without significant limitations.
Similarly, John, a retired teacher, discovered his condition during a routine check-up. By following a structured treatment plan and staying active, he enjoys his retirement, staying engaged in community activities. Their stories exemplify the possibility of leading a normal, healthy life with myocarditis.
Incorporating the ‘HEART’ strategies into daily routines provides a robust framework for both preventing myocarditis and thriving post-diagnosis. It fosters hope and underscores the power of proactive health management.