Introduction to Endocarditis
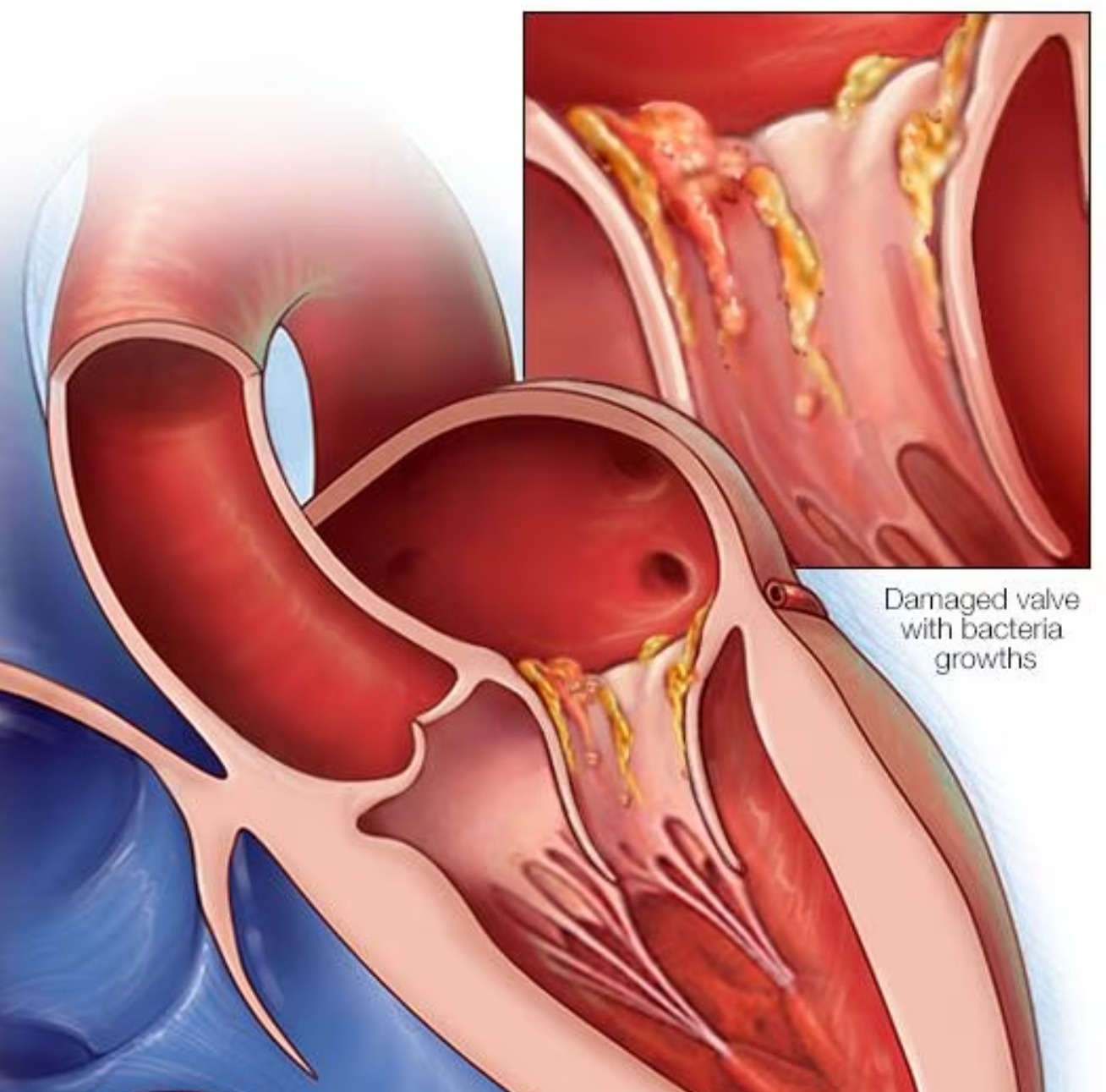
Imagine your heart as the home you live in, a place designed to function smoothly and keep you healthy. Now, picture an unexpected guest arriving and creating chaos in your home – that’s akin to what happens with endocarditis in the heart. Endocarditis is a serious condition characterized by the inflammation of the inner lining of the heart, particularly affecting the heart valves. It can be caused by bacteria, fungi, or other microorganisms entering the bloodstream and attaching themselves to damaged areas of the heart. Just like an unwelcome guest causing trouble in your home, these infectious agents disrupt the normal functioning of the heart.
Understanding endocarditis is crucial for both healthcare professionals and individuals without a medical background. This condition, while not common, carries significant risks and can lead to serious complications if left untreated. Medical practitioners deal with endocarditis cases regularly and are aware of the detailed clinical aspects, treatment protocols, and preventive measures. For the general population, having a basic understanding helps in recognizing symptoms early and seeking prompt medical care.
This guide aims to demystify endocarditis, making the topic approachable for everyone. We will explore what endocarditis is, how it affects the heart, the causes behind it, the symptoms to watch for, and the ways it can be treated or prevented. Whether you are a doctor looking to refine your knowledge or someone curious about their health, this blog post will provide a comprehensive overview of endocarditis. So, let’s delve deeper and address this hidden adversary that can potentially turn one’s heart from a serene haven to a battleground.
Causes and Risk Factors
Endocarditis is an infection of the inner lining of the heart, typically caused when bacteria, fungi, or other germs enter the bloodstream and attach to damaged areas of the heart. Understanding the primary causes and recognizing the risk factors are crucial for both prevention and early diagnosis. Three primary sources can lead to endocarditis: bacteria, fungi, and other infectious agents. These microorganisms can enter the bloodstream through various routes, including dental procedures, surgical interventions, or even minor cuts and scrapes that become infected.
To remember the risk factors associated with endocarditis, we can utilize the mnemonic ‘BAD VALVES’:
-
Bacteria: The most common cause is a bacterial invasion, particularly from Streptococci or Staphylococci species.
-
Artificial heart valves: People with prosthetic heart valves are at higher risk as these can provide surfaces for bacteria to adhere to and cause infection.
-
Dentistry issues: Poor dental hygiene or invasive dental procedures can introduce bacteria into the bloodstream.
-
Valve disease: Those with pre-existing conditions such as rheumatic heart disease or mitral valve prolapse are more susceptible.
-
Aging: As people age, their risk increases due to potential degenerative changes in the heart and valves.
-
Lovers (drug users): Intravenous drug use can introduce bacteria directly into the bloodstream, raising the risk of endocarditis.
-
Every heart condition: Congenital heart defects or previous episodes of endocarditis increase susceptibility.
-
Sepsis: Severe blood infections can result in the spread of bacteria to the heart, causing endocarditis.
For instance, everyday activities such as brushing teeth or minor injuries can lead to bacteremia, especially if proper hygiene is not maintained. People with dental issues or those who undergo invasive procedures without appropriate prophylactic measures face higher risks. Additionally, individuals with existing heart conditions or prosthetic valves should exercise caution during medical procedures and maintain rigorous hygiene practices to minimize the chances of contracting endocarditis.
Signs and Symptoms
Endocarditis, despite being an intricate medical condition, often manifests with symptoms that might resemble more familiar illnesses, making it challenging to identify. Among the initial signs that individuals may experience is an unexplained fever. Picture waking up with a temperature that won’t go away, despite not having a cold or flu. This persistent fever can be an early warning sign of endocarditis.
Accompanying this fever, individuals may endure chills comparable to the shivers experienced on a particularly cold day. One might assume these chills are just part of feeling under the weather, but when combined with other symptoms, they could suggest something more serious. Another common symptom is an unusual level of fatigue or feeling extremely tired without exertion. Imagine feeling drained of energy after simple tasks, like making breakfast or taking a short walk. This level of tiredness, coupled with other signs, cannot be overlooked.
The phrase “Fever and chills give me thrills, but pain in the chest is no jest” can serve as a helpful mnemonic to remember these warning signs. Some individuals with endocarditis might also notice chest pain, which is a clear red flag. This pain can intensify with breathing or occur sporadically, presenting an urgent need for medical attention.
A less common but notable symptom includes tiny purple or red spots on the skin, particularly on the fingers or toes, known as Janeway lesions. Visualize these as small bruises that appear without an obvious cause. Another potential sign is night sweats, waking up drenched in sweat as if you had been running a marathon in your dreams.
Real-life scenarios illustrate how these symptoms might unfold. Imagine a busy individual, constantly on the go, suddenly finding themselves frequently fatigued, unable to shake off an unexplainable fever, and waking up in a sweat each night. These subtle, yet persistent symptoms may all point towards endocarditis, necessitating a visit to a healthcare professional for a thorough examination.
Recognizing these signs in oneself or a loved one can be crucial. Early detection and prompt medical attention are vital to managing endocarditis effectively. Therefore, understanding these symptoms is a significant step towards promoting better health and well-being.
Diagnosis and Tests
Diagnosing endocarditis involves a series of tests aimed at identifying the infection and its impact on the heart. Given the critical nature of the condition, doctors employ a systematic approach, simplified here for easy understanding.
The first and often most crucial test is the blood culture. Think of it as taking a sample to identify what’s causing trouble in your body. Blood cultures are like a detective’s toolkit, where the blood is examined for bacteria or fungi over a specified period. If the blood “grows” microorganisms, it indicates an infection, helping doctors determine the specific culprit and guide appropriate treatment.
Another essential test is the echocardiogram, abbreviated as an “ECHO.” This is akin to an ultrasound, which uses sound waves to create detailed images of your heart. These images help doctors see the heart valves and chambers, pinpointing any abnormal growths or infections that signify endocarditis. There are two types of echocardiograms: transthoracic (TTE) and transesophageal (TEE). While TTE is performed outside the chest, TEE involves a probe inserted down the throat to get closer images of the heart.
To remember these key tests, think of the rhyme: “ECHO shows, BLOOD grows.” This mnemonic can be a simple and effective way to recall the primary measures taken to diagnose endocarditis.
In addition to blood cultures and echocardiograms, doctors might order other tests such as complete blood counts (CBC), chest X-rays, or electrocardiograms (EKG) to gather more information about the heart’s condition and the extent of the infection. These comprehensive diagnostics ensure that endocarditis is accurately identified and appropriately managed.
Understanding these diagnostic tools can demystify the process and highlight the importance of timely and thorough testing when endocarditis is suspected. Early and precise diagnosis paves the way for prompt and effective treatment, crucial in addressing this serious condition.
Treatment Options
Treating endocarditis often calls for a careful and precise approach, akin to fixing a complex machine. The primary method involves antibiotics to fight the underlying infection, the “critters” causing the illness – hence the rhyme: “Antibiotics for the critters, surgery if it quivers.” This simple rhyme helps remember that while medicines are the first line of defense, more severe cases might need surgical intervention.
When a patient is diagnosed with endocarditis, doctors typically start by prescribing a course of antibiotics. These medications target and eliminate the bacteria, much like how we use special tools to repair machinery or, in simpler terms, take the right medicine for everyday infections. The chosen antibiotics depend on the bacteria causing the infection, identified through blood tests. Administered intravenously (IV) for more extended periods, commonly four to six weeks, this aggressive approach is critical to ensure the complete eradication of the bacterial menace.
However, in some cases, the damage inflicted by the infection is extensive. Here, surgical solutions come into play, especially when heart valves – the essential parts of our “engine” – are severely damaged and cannot function normally. Surgery aims to repair or replace these damaged heart valves, similar to replacing parts in a car that no longer work efficiently. For example, minimally invasive surgery has shown successful outcomes, involving small incisions and specialized instruments to repair the damage whilst reducing recovery time and promoting better outcomes.
The immediate intervention is pivotal. Timely medical assistance can make a significant difference between a complete recovery and complex, life-threatening complications. Medical records have ample instances where prompt antibiotic treatment coupled with well-timed surgical procedures restored patients to full health. Mary’s case is a testimonial: diagnosed early, she underwent a rigorous antibiotic regimen followed by surgery to replace a damaged heart valve, leading to a smooth recovery.
Endocarditis treatment exemplifies modern medicine’s capabilities, combining advanced pharmacology and surgical ingenuity. Following the rhythm of timely intervention, appropriate antibiotics, and necessary surgeries can navigate through the turbulence caused by endocarditis, ensuring smoother, healthier outcomes for patients.
Prevention and Lifestyle Adjustments
Endocarditis, though a serious condition, can often be prevented through diligent lifestyle choices and proactive routines. A mnemonic such as ‘CLEAN TEETH’ can serve as a helpful guide to remember key preventive measures:
Carry on hygiene: Maintaining strict dental hygiene is crucial. Brushing and flossing regularly reduces the risk of bacteria entering the bloodstream through inflamed gums. Remember, the mouth is a gateway to overall health.
Limit risks: Avoid behaviors that increase the risk of infection such as intravenous drug use. Ensure medical procedures are only done with sterile equipment.
Eat healthily: A balanced diet strengthens the immune system, helping the body fend off infections that might lead to endocarditis.
Avoid risky behaviors: Be cautious with body piercings and tattoos, which can introduce harmful bacteria into the bloodstream. Always ensure these procedures are performed in a sterile environment.
Notice symptoms: Pay attention to symptoms like persistent fever, fatigue, or unexplained weight loss. Early detection of such symptoms may significantly mitigate risks.
Take regular checkups: Regular medical and dental checkups are essential in catching potential issues early. Discuss any concerns or symptoms with your healthcare provider during these visits.
Everyday care: Small daily habits, such as washing hands often and avoiding contact with sick individuals, contribute significantly to general health and infection prevention.
Eliminate germs: Disinfection and maintaining cleanliness in personal and shared spaces reduce the chances of bacterial invasion. Simple actions like cleaning surfaces regularly can prevent the spread of harmful microorganisms.
Treat issues early: Addressing health problems promptly, before they escalate, is central in preventing endocarditis. Timely, effective treatment of infections such as strep throat can stop bacteria from spreading to the heart.
Help and heed advice: Follow medical advice diligently and don’t hesitate to seek help if needed. Professional guidance tailored to individual health needs can make a significant difference in prevention.
Consider Sarah, a university student who recently noticed bleeding gums. By adhering to the ‘CLEAN TEETH’ mnemonic, she not only sought timely dental care but also made lifestyle adjustments to avoid future complications. Such practical steps sometimes mean the difference between health and potential heart issues.