What is Sepsis?
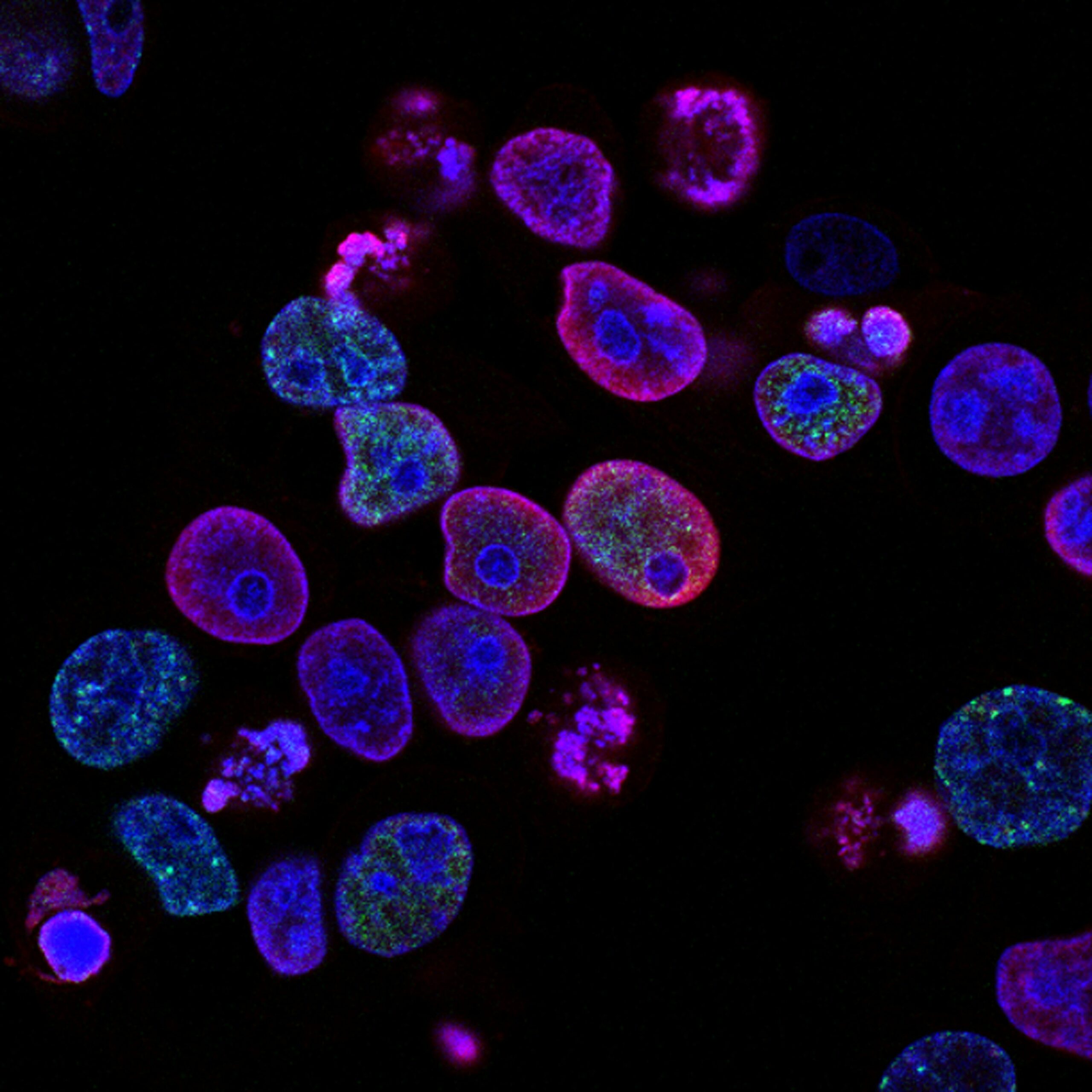
Sepsis is a critical and potentially life-threatening condition that arises when the body’s response to an infection triggers widespread inflammation. This severe reaction can be caused by various pathogens including bacteria, viruses, fungi, or parasites. When the body detects an infection, it releases chemicals into the bloodstream to fight off the invading pathogens. However, in the case of sepsis, this response becomes dysregulated, leading to a series of complications that can harm organs and tissues, ultimately putting the individual’s life at risk.
To understand sepsis more clearly, consider a common scenario: a person with a cut or a minor infection, such as pneumonia. Under normal circumstances, the body efficiently handles these infections through a localized immune response. However, in some cases, the immune response can spiral out of control. This cascade of inflammation may result in fever, rapid heart rate, difficulty breathing, and confusion – all signs that something has gone awry. If untreated, sepsis can progress to septic shock, a more severe state characterized by drastically low blood pressure and high mortality rates.
The reason sepsis is often termed a ‘silent killer’ is due to its insidious nature. Early symptoms may be mistaken for less serious conditions, leading to delays in diagnosis and treatment. Furthermore, the risk factors for developing sepsis include age, chronic illnesses, recent surgeries, or immunocompromised states, making it important for those at risk to be vigilant. Recognizing the signs of sepsis early on can significantly improve outcomes. It is crucial for individuals and healthcare professionals alike to be aware of the symptoms and act swiftly, as timely intervention can be the difference between life and death. Are you a nurse, nursing student, medical doctor, medical student, or other health allied professional? Or perhaps a curious individual wanting an in-depth understanding of sepsis for examination, clinical practice, or knowledge? Then kindly check out my book, Understanding Sepsis: The Silent Killer Demystified, available on Gumroad. For more details, click the link above. However, feel free to read below for general information.
How Sepsis Develops
Sepsis originates from a localized infection that has the potential to escalate into a systemic response, affecting the entire body. Common triggers of sepsis include pneumonia, urinary tract infections, and skin infections. Typically, these infections start in a specific area and provoke a response from the immune system. The body, in an effort to fight the pathogenic microorganisms, releases chemicals into the bloodstream. This response aims to contain and eradicate the infection but can inadvertently lead to widespread inflammation.
Initially, the immune system’s reaction is beneficial; however, as the infection spreads, it can result in an overreaction known as a “cytokine storm.” This excessive release of inflammatory markers can cause blood vessels to become increasingly permeable, leading to fluid leakage into the surrounding tissues. Consequently, organs may begin to suffer from inadequate blood flow, which can impair their function significantly. Given the complexity of this cascade, it’s essential to understand the stages of sepsis: sepsis, severe sepsis, and septic shock.
In the first stage, known simply as sepsis, an infection is identified, and the body shows early signs of systemic inflammation. This may manifest as a high fever, increased heart rate, or rapid breathing. As the condition progresses to severe sepsis, the body’s ability to cope diminishes, leading to organ dysfunction. If timely medical intervention is not sought, the final stage, septic shock, may occur, which is characterized by critically low blood pressure and multiple organ failure. Hence, recognizing the early signs of sepsis is crucial, as prompt treatment can significantly increase survival rates and improve outcomes.
Recognizing the Symptoms of Sepsis
Sepsis is a serious medical condition that arises when the body’s response to an infection causes widespread inflammation. Early detection of sepsis can significantly improve outcomes, making it essential for individuals to be aware of its symptoms. Symptoms can vary depending on the stage of sepsis and can be categorized into mild, moderate, and severe stages.
In the initial stage, known as sepsis, some common symptoms include fever, chills, increased heart rate, rapid breathing, and confusion. These symptoms may be mistaken for a common infection or flu, which can lead to delays in seeking appropriate treatment. Individuals may also experience weakness, unusual pains, or malaise, which serve as critical warning signs that should not be overlooked.
As sepsis progresses to moderate or severe stages, symptoms may escalate in severity. In cases of severe sepsis, the individual may exhibit signs of organ dysfunction. Symptoms may include shortness of breath, significant drop in blood pressure, decreased urine output, and altered mental status. Confusion can become more pronounced, leading to a state of delirium or unconsciousness. At this stage, urgent medical intervention is crucial to prevent potential complications.
Finally, septic shock represents the most severe stage of sepsis. It is characterized by persistent hypotension despite adequate fluid resuscitation, resulting in severe organ failure. Symptoms in this stage may include a bluish coloration of the skin, cold extremities, and significant confusion or disorientation. Recognizing these symptoms promptly can be lifesaving and underscores the importance of immediate medical attention.
In conclusion, understanding the symptoms of sepsis at various stages is vital for early recognition and intervention. Staying informed can empower individuals to seek timely medical care, ultimately reducing the risks associated with this potentially life-threatening condition.
Risk Factors and Vulnerable Populations
Sepsis is a serious medical condition that can develop in anyone, but certain groups of individuals are at a higher risk. Understanding these risk factors is crucial in recognizing and preventing severe outcomes associated with this condition. One of the primary demographic factors influencing susceptibility to sepsis is age. Older adults, particularly those aged 65 and above, are significantly more vulnerable due to natural declines in immune function, increased likelihood of chronic diseases, and often, the presence of frailty, which complicates their overall health status.
Chronic illnesses also play a significant role in elevating sepsis risk. Individuals living with conditions such as diabetes, heart disease, lung disease, or cancer frequently experience compromised immune systems. These health issues can make it more challenging for the body to fight off infections, thereby increasing the likelihood of sepsis development. Additionally, patients undergoing immunosuppressive treatments, whether for autoimmune diseases or as part of cancer therapies, are particularly prone to infections that can escalate into sepsis.
Another critical factor is recent surgical interventions. Individuals who have undergone surgery, particularly invasive procedures, may have an increased risk of developing infections. Surgical sites and internal body cavities can become entry points for pathogens. Furthermore, hospitalization itself can increase exposure to bacteria and other pathogens, particularly in environments where antibiotic-resistant infections may occur. As a result, understanding these risk factors allows vulnerable populations to be more proactive in their care. The implementation of infection prevention strategies and timely medical interventions can be critical steps in managing the risks associated with sepsis.
The Importance of Early Detection
Sepsis remains a life-threatening condition that arises when the body’s response to an infection spirals out of control, potentially leading to organ failure and death. The significance of timely diagnosis and treatment of sepsis cannot be overstated, as early intervention plays a crucial role in improving outcomes for affected individuals. According to research, the chances of surviving sepsis decrease significantly with every hour that treatment is delayed. For instance, patients who receive appropriate treatment within the first hour of showing symptoms have a mortality rate of approximately 20%, whereas this figure rises to 40% if treatment is delayed by just a few hours.
The prompt identification of sepsis symptoms is essential, as they can vary widely among patients. Common indicators include a rapid heart rate, elevated body temperature, or unusual confusion. Recognizing these warning signs as part of a broader clinical approach can facilitate quicker clinical decision-making. Timely intervention not only improves patient survival rates but also minimizes the risk of long-term complications, such as post-sepsis syndrome, which can affect quality of life.
Personal stories of sepsis survivors further highlight the importance of early detection. Take, for example, the story of a 35-year-old man who developed sepsis after a routine surgery. Due to a lack of awareness regarding the symptoms, he initially dismissed his fever and fatigue. It was only after his family insisted on seeking immediate medical attention that he received appropriate treatment. His experience demonstrates how critical awareness is, not just within healthcare settings, but also among patients and their families.
Overall, the focus on early detection of sepsis is paramount in combating this silent killer. Efforts to educate both the public and healthcare professionals about the signs and symptoms of sepsis can lead to better recognition and faster medical response, ultimately saving lives and improving health outcomes.
Diagnosis: How is Sepsis Identified?
Diagnosing sepsis is a crucial and often complex process that requires a comprehensive evaluation of the patient. Healthcare professionals typically begin by conducting a detailed medical history and physical examination to assess symptoms. Common indicators of sepsis include fever, rapid heart rate, confusion, and difficulty breathing. However, because these symptoms can overlap with other conditions, further diagnostic tests are usually necessary.
One of the primary tools used in diagnosing sepsis is blood testing. A complete blood count (CBC) can reveal elevated white blood cell counts, which often signify an infection. Blood cultures are also crucial since they identify the specific bacteria or fungi causing the infection. Additionally, blood tests can measure lactate levels, which rise in cases of tissue hypoperfusion, a condition that frequently occurs in septic patients.
Moreover, healthcare providers may utilize imaging studies to determine the source of infection. Imaging techniques, such as X-rays, ultrasounds, or CT scans, serve to visualize potential infection sites, including abscesses, pneumonia, or other related complications. Early identification of these sources can significantly influence the treatment approach.
Further, physicians may assess organ function as sepsis can lead to organ dysfunction, a key component in the severity of the illness. Tests that evaluate liver enzymes, kidney function, and coagulation parameters help in understanding the extent of sepsis’s impact on the body.
In conclusion, the identification of sepsis involves a multifaceted approach, integrating patient history, physical examination, blood tests, and imaging studies. This comprehensive method ensures prompt diagnosis, which is crucial for effective treatment and improving patient outcomes. Understanding the diagnostic procedure enhances appreciation for the timely actions taken in healthcare settings to combat this serious condition.
Treatment Options for Sepsis
Sepsis is a medical emergency that requires prompt treatment to improve the chances of survival and minimize complications. The cornerstone of sepsis management is the early administration of antibiotics. Upon diagnosis, a healthcare provider typically initiates broad-spectrum antibiotics, targeting a range of possible bacteria. This immediate action is crucial as delays in the initiation of appropriate antibiotics can increase morbidity and mortality rates associated with sepsis.
In addition to antibiotics, intravenous (IV) fluids play a vital role in managing sepsis. Patients often experience significant fluid loss and low blood pressure due to the systemic inflammatory response. Therefore, administering IV fluids helps restore adequate circulation, ensuring that vital organs receive sufficient oxygen and nutrients. The choice of fluids, which can include saline or lactated Ringer’s solution, depends on the patient’s condition and specific medical needs.
Another fundamental aspect of treatment involves monitoring and supporting organ function. In severe cases, patients may require medications to support blood pressure and improve heart function. Vasopressors are commonly used to elevate blood pressure when IV fluids alone are insufficient. In some scenarios, additional interventions may be necessary, such as mechanical ventilation if respiratory support is required.
Alongside these interventions, some patients may benefit from adjunctive therapies aimed at modulating the immune response or preventing complications. For example, corticosteroids can be considered for specific cases of septic shock, but their use depends on individual patient factors. Regular monitoring in an Intensive Care Unit (ICU) setting is often warranted to address evolving clinical challenges effectively.
Overall, the treatment of sepsis is multifaceted, involving a combination of antibiotics, fluid resuscitation, and supportive care tailored to the patient’s specific situation. Understanding these treatment modalities can empower patients and their families to engage actively in discussions regarding their care when faced with this critical condition.
Preventing Sepsis: Tips and Best Practices
Preventing sepsis is crucial in reducing its incidence and associated morbidity. The strategies for preventing this serious condition largely focus on maintaining good hygiene practices, staying updated on vaccinations, and effectively managing chronic health issues. Each of these areas plays a vital role in minimizing the risk of infections that can lead to sepsis.
Firstly, personal hygiene should not be underestimated. Regular handwashing with soap and water is one of the most effective ways to prevent many infections. This practice becomes even more important in healthcare settings, where exposure to pathogens is higher. Individuals should also be mindful of taking care of any cuts or wounds by cleaning them properly and covering them with sterile dressings to prevent infection. Adopting good hygiene not only protects oneself but also those around them, thus contributing to community health.
Another critical factor in preventing sepsis is vaccination. Vaccines play a significant role in protecting against various infectious diseases, which can lead to sepsis. For instance, vaccinations for pneumonia, influenza, and meningococcal disease significantly reduce the incidence of related infections. It is essential to stay current with recommended vaccinations, particularly for individuals in high-risk groups, such as the elderly or those with compromised immune systems.
Furthermore, managing chronic health concerns, such as diabetes or autoimmune disorders, plays an essential role in preventing infections. Proper management of chronic conditions through regular medical check-ups, following treatment plans, and making lifestyle adjustments can help mitigate infection risks. Patients should communicate openly with their healthcare providers about any changes in their health status, ensuring comprehensive care that targets not just the chronic condition but also its potential complications.
Through the implementation of these best practices—maintaining hygiene, staying vaccinated, and managing chronic illnesses—individuals can significantly decrease their risk of developing sepsis. Awareness and proactive measures are key components in the fight against this often-overlooked condition.
Living After Sepsis: Recovery and Long-Term Effects
Experiencing sepsis can be a life-altering event, impacting not only the individual’s physical health but also their emotional well-being. The recovery process from sepsis varies considerably among patients, depending on the severity of the illness and underlying health issues prior to the infection. While some individuals may resume their daily activities within weeks, others may face a prolonged journey to recovery.
One significant concern for survivors is the potential for post-sepsis syndrome (PSS). This condition can manifest in various forms, including physical, psychological, and cognitive effects, which may linger for months or even years. Survivors might experience fatigue, sleep disturbances, muscle pain, and joint problems. Cognitively, issues such as memory loss, difficulty concentrating, and anxiety are also common. Psychological effects can range from depression to post-traumatic stress disorder (PTSD), influenced by the traumatic experience of sepsis and its treatment.
Follow-up care is a crucial aspect of the recovery journey. Engaging regularly with healthcare providers enables survivors to monitor their progress, manage lingering symptoms, and receive appropriate rehabilitation to regain strength and functionality. Physical therapy can play a vital role in helping individuals rebuild endurance and mobility, while mental health support, such as counseling or support groups, can aid emotional healing.
Despite the challenges associated with recovery from sepsis, it is essential to highlight the hope and support available. Many resources, including dedicated sepsis organizations, provide valuable information, advocacy, and community for survivors and their families. Building a robust support system among friends, family, and healthcare professionals can significantly enhance the recovery experience.
Ultimately, while the aftermath of sepsis can be daunting, understanding the potential long-term effects and having access to appropriate support and resources is pivotal for a successful recovery. Survivors can reclaim their lives and find new meaning in their journey beyond sepsis.